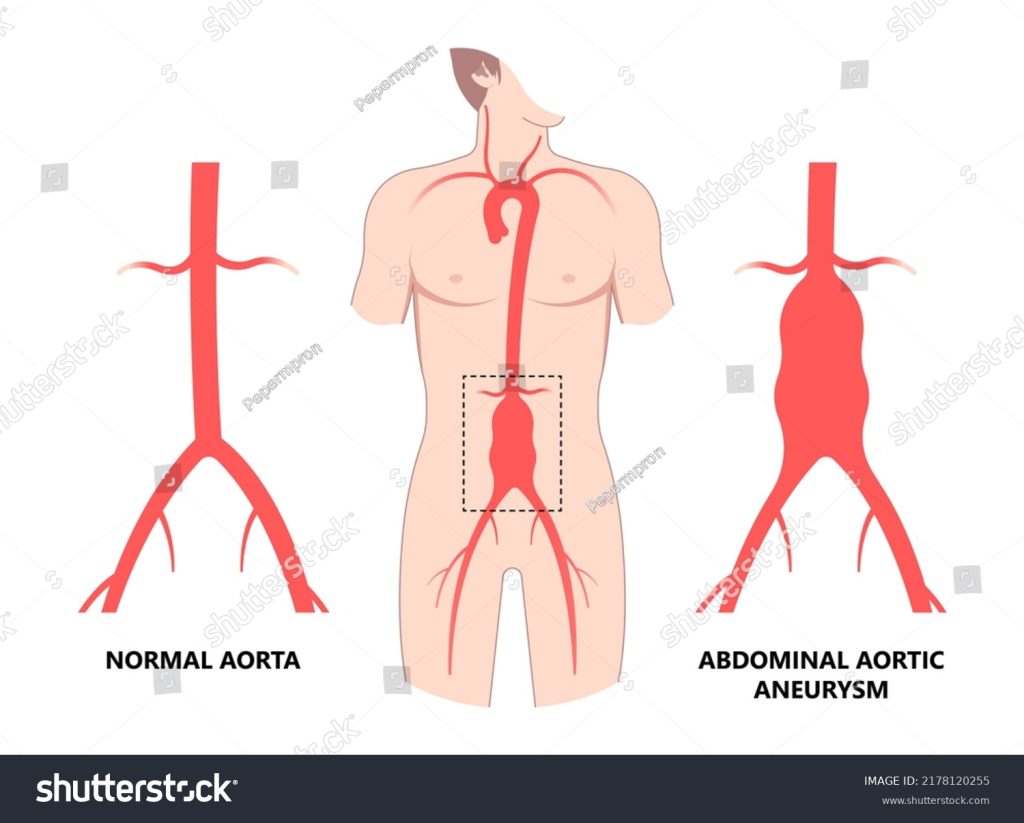
Abdominal Aortic Aneurysm
Abdominal aortic aneurysm (AAA) is more common in men over 65 and smokers. If it ruptures, it is very dangerous, with more than 80% of cases being fatal. Detecting AAA early can improve treatment outcomes, with options including monitoring, lifestyle changes, or surgery. Timely intervention significantly reduces health risks and saves lives.
Overview
An abdominal aortic aneurysm is a localized bulging or enlargement of the abdominal aorta, the largest artery in the body, which carries blood from the heart to the rest of the body. It occurs when a section of the aorta weakens and expands, posing a risk of rupture. Often asymptomatic, a ruptured AAA can cause life-threatening internal bleeding. Early detection through regular check-ups and screenings is vital for managing the condition and preventing complications.
Types of Abdominal Aortic Aneurysm
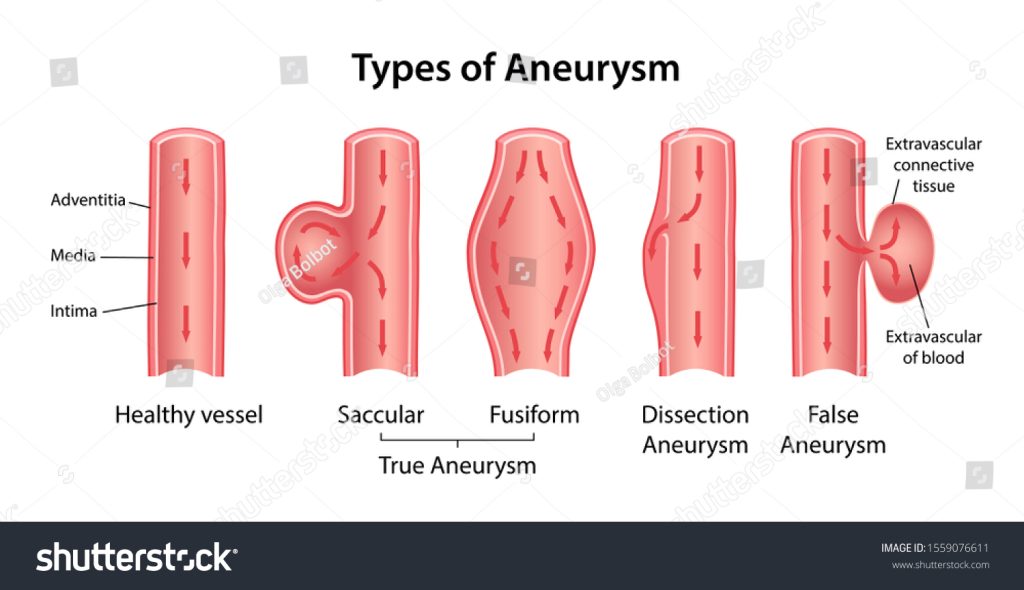
| Type | Description | Prognosis | Symptoms |
|---|---|---|---|
| Fusiform Aneurysm | Fusiform aneurysms are the most common type. They affect the entire circumference of the artery, leading to a uniform, tube-like swelling. | The prognosis varies with size; larger aneurysms have a higher risk of rupture. | Often asymptomatic Pulsating feeling near the navel Deep, constant pain in the abdomen or side of the abdomen Back pain |
| Saccular Aneurysm | Saccular aneurysms appear as a localized, balloon-like bulge on one side of the artery wall. | These aneurysms are more prone to rupture, especially if they grow rapidly. Require monitoring and possibly surgical intervention. | Potentially asymptomatic Severe pain in the back or abdomen Pain that radiates to the legs or buttocks |
| Dissecting Aneurysm | A dissecting aneurysm occurs when there is a tear in the inner layer of the aorta, causing blood to flow between the layers of the artery wall. | High risk of rupture or blockage and generally requires emergency surgical treatment. | Sudden, severe, and persistent chest or back pain Pain that feels like it’s tearing or ripping Shortness of breath |
When to See a Doctor
The main complications of a thoracic/abdominal aortic aneurysm(AAA) are aortic wall tears and rupture. While small, slow-growing aneurysms may not rupture, larger aneurysms carry a higher risk. If untreated, AAA can lead to severe pain and further complications like:
- Internal Bleeding:
Life-threatening and requires immediate emergency surgery - Aortic Dissection:
A tear in the aortic wall, leading to severe pain and possible rupture. - Blood Clots:
Blod clots can form and potentially block blood flow to other organs or limbs. - Compression:
A growing aneurysm may press on nearby structures, causing pain or organ dysfunction. - Reduced Blood Flow:
This can disrupt normal blood flow, leading to organ damage or ischemia in affected areas. - Infection:
Rarely, an aneurysm may become infected, causing fever, pain, and systemic illness - Aortoenteric fistula (AEF):
A rare but serious complication where an abnormal connection forms between the aorta and the gastrointestinal tract, usually the duodenum.
Timely treatment is critical to avoid these potentially fatal outcomes.

Emergency Situations
An abdominal aortic aneurysm (AAA) is a serious condition that can become life-threatening if not addressed promptly. Seek immediate emergency medical help if you experience:
- Sudden, severe, and persistent abdominal or back pain.
- Pain that radiates to the back or legs.
- Symptoms of shock, such as rapid pulse, cold, clammy skin, and confusion.
- A known AAA with new or worsening symptoms.
If you suspect a rupture, call emergency services immediately or go to the nearest hospital’s emergency department.
Routines for Pre-existing Conditions
If you have been diagnosed with an abdominal aortic aneurysm, regular routine checkups are crucial for monitoring the condition:
- Small AAAs (3.0 – 4.0 cm): Require ultrasound or CT scan every year, as advised by your doctor.
- Medium AAAs (4.0 – 5.5 cm): Typically need monitoring every 6 – 12 months, depending on how fast it develops and based on your doctor’s recommendation.
- Large AAAs (> 5.5 cm): Might require more frequent assessments or surgical intervention.
- An annual routine check-up is necessary to monitor related underlying health conditions, such as blood pressure and diabetes, and to adjust medications as needed.
Early detection of AAA can significantly reduce the risk of rupture, which has a high mortality rate. Routine checkups and imaging can lead to timely interventions, such as surgery or endovascular repair, to prevent life-threatening complications. Consult with a vascular surgeon or a cardiologist for appropriate management and follow-up schedules.
Preventative Checkups Based on Family History or Lifestyle Factors
Preventative early screening and regular monitoring may be beneficial for certain individuals based on family history and lifestyle risk factors(such as smoking, high blood pressure, or older age):
- Men aged 65 – 75 who have smoked should have a one-time ultrasound to check for an AAA.
- Individuals with a family history of AAA should discuss screenings with their doctor, potentially starting at an earlier age than typically recommended.
- People with risk factors such as high blood pressure, high cholesterol, or atherosclerosis should consider more frequent checkups as advised by their healthcare provider.
Doctors to Consult
For diagnosis, monitoring, and treatment of an abdominal aortic aneurysm, consult with:
- Vascular Surgeon: Expert in conditions and surgeries related to the blood vessels.
- Cardiologist: May assist with cardiovascular risk factors and provide guidance on medical treatment.
- Radiologist: Conducts and interprets imaging tests such as ultrasounds, CT scans, or MRIs to evaluate the aneurysm’s size and condition. Radiologists are typically involved indirectly during diagnostic or monitoring imaging.
- Interventional Radiologist: Focuses on minimally invasive procedures like endovascular aneurysm repair (EVAR) and collaborates with vascular surgeons for nonsurgical treatments.
- General Physician: Helps coordinate overall healthcare and referrals to specialists for imaging and follow-ups.
Risk Factors/Causes
The exact cause of an abdominal aortic aneurysm is not always clear, but several factors can increase the risk of developing one.
Family History & Genetics
- Family history of abdominal aortic aneurysm (AAA)
- Genetic disorders such as Marfan syndrome and Ehlers-Danlos syndrome
Age & Sex
- Risk increases significantly after 65 years
- Males are at higher risk compared to females
- Caucasians have a higher risk of AAA compared to other races, including African Americans. South Asians, while at lower direct risk for AAA, have higher rates of diabetes, hypertension, and dyslipidemia – key cardiovascular risk factors – highlighting the need for proactive management to reduce vascular complications.
Lifestyle Habits
- Smoking: The leading risk factor for AAA development.
- Unhealthy Diet: Diets rich in cholesterol and fats can damage arteries.
- Excessive Alcohol Consumption: Increases cardiovascular risks.
- Physical Inactivity: Sedentary lifestyles elevate risks such as high blood pressure.

Pre-existing Medical Conditions
- Hypertension: High blood pressure can damage the blood vessels and lead to aneurysms.
- Atherosclerosis: The buildup of plaques in the artery walls can weaken them, raising the risk.
- Peripheral vascular disease: Conditions affecting blood flow can contribute to aneurysm formation.
- Chronic obstructive pulmonary disease (COPD): This condition may be associated with an increased risk.
Prevention of AAA
- Quit Smoking:
Smoking is a major risk factor for the development of an abdominal aortic aneurysm. Quitting smoking can significantly reduce your risk. - Control Blood Pressure:
High blood pressure can weaken the aortic walls and contribute to aneurysm formation. Regular monitoring and management through lifestyle changes or medication can aid in prevention. - Manage Cholesterol Levels:
High cholesterol can contribute to atherosclerosis, which can weaken the aorta. Maintaining healthy cholesterol levels through diet, exercise, and medications can help. - Control diabetes:
If you have diabetes, managing your blood sugar levels can help reduce the risk of complications that may contribute to aneurysm formation.
- Eat a Healthy Diet:
Consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to maintain optimal cardiovascular health. - Exercise Regularly:
Regular physical activity can help maintain a healthy weight, lower blood pressure, and reduce aneurysm risk. - Regular Check-ups:
If you are at risk, screen regularly, especially for men over 65 and those with a family history of aneurysm. Early detection can lead to timely treatment. - Maintain a Healthy Weight:
Obesity increases your risk of developing multiple health issues, including aneurysms, due to additional strain on your heart and blood vessels.

- Limit Alcohol Intake:
Excessive drinking can lead to high blood pressure. Limit your intake to moderate levels. - Attend regular health check-ups:
Routine check-ups with your healthcare provider can help detect any potential issues early and allow for proactive management. - Know your family history:
Be aware of your family medical history, as a genetic predisposition can increase your risk; discuss this with your doctor if applicable.
Diagnosis
Diagnosing an Abdominal Aortic Aneurysm (AAA) involves a combination of physical examinations, imaging studies, and laboratory tests. The following is a detailed overview of the diagnostic process and the order of medical evaluations typically performed:
Medical History and Physical Examination
Initial evaluation often includes a thorough medical history and physical examination. Clinicians may assess symptoms such as back or abdominal pain and look for physical signs of an aneurysm, like unusual abdominal masses or pulsation.
Laboratory Tests
While laboratory tests cannot directly diagnose AAA, they are crucial for assessing overall health and ensuring surgical readiness.
- Complete Blood Count (CBC): Screens for anemia or infection.
- Basic Metabolic Panel (BMP): Evaluates kidney function and electrolyte levels.
- Coagulation Profile (INR/PT/PTT): Checks blood clotting function.
- Lipid Profile: Identifies cardiovascular risk factors.
- Serum Creatinine and Blood Urea Nitrogen (BUN): Monitors kidney function, which is especially important if contrast dye imaging is needed.
- Electrolyte Panel: Ensures proper balance of sodium, potassium, and other essential minerals.
- Liver Function Tests: Assesses liver health as part of pre-operative evaluation.

Urinalysis
- Performed to detect infections or abnormalities as part of surgical preparation.
Imaging and Functional Tests

If an AAA is suspected from the clinical evaluation, imaging tests are crucial to confirm the diagnosis and assess the aneurysm’s size and location. Common imaging tests include:
- Abdominal Ultrasound: This is usually the first imaging test used to confirm the presence of an AAA due to its convenience and non-invasive nature. It can accurately measure the size of the aneurysm.
- Normal: Aorta is under 3 cm, and no issues were detected.
- Small Aneurysm: 3 – 4.4 cm; requires monitoring.
- Medium Aneurysm: 4.5 – 5.4 cm; needs regular follow-ups.
- Large Aneurysm: 5.5 cm or more; high rupture risk; surgery may be needed.
- Rapid Growth: Growth over 0.5 cm in 6 months; immediate attention required.
Your doctor will guide you based on the size and growth of the aneurysm.
- Abdominal Computed Tomography (CT) Scan: A CT scan with contrast is often employed to provide a more detailed image of the aneurysm and its anatomical relationships. It is often used for a detailed evaluation when an AAA is suspected to be large or when surgery is being considered.
- Abdominal Magnetic Resonance Imaging (MRI): Rarely used as the first-line test but can provide detailed images of blood vessels and be useful in planning surgical interventions. MRI uses a magnetic field and radio waves and is used in certain cases to provide further anatomical details of abdominal structures, especially if there’s a contraindication to using contrast in the CT scan.
- Abdominal CT Angiography(CTA): CTA is the gold standard for evaluating AAAs, especially before surgery. It helps define vascular anatomy for surgical or endovascular repair. Contrast dye is injected, and cross-sectional images are captured to create detailed 3D reconstructions.
Emerging Tests
- Specific Biomarkers:
Research is ongoing to identify blood markers that may predict aneurysm presence or rupture risk, but these are not yet part of standard practice.
Risk Assessment and Monitoring
- Aneurysm Size and Growth Monitoring: If an AAA is detected, monitoring over time is essential to determine the risk of rupture. This often involves regular ultrasound or CT imaging based on the aneurysm size and growth rate.
- Cardiovascular Risk Assessment: Further evaluation might be conducted to assess and mitigate other cardiovascular risks that may impact overall treatment decisions.
In conclusion, diagnosing an abdominal aortic aneurysm is a multi-step process that involves a comprehensive assessment using clinical evaluation, imaging, and laboratory tests to guide management and treatment decisions.
Allopathic Treatment
The treatment for an abdominal aortic aneurysm (AAA) in allopathic medicine largely depends on the size and rate of growth of the aneurysm, as well as the patient’s symptoms and overall health condition. The main treatment strategies include surveillance, medication, and surgery:
Surveillance
If the aneurysm is small and does not cause any symptoms, the doctor may recommend regular monitoring through imaging studies like ultrasound or CT scans. The frequency of monitoring depends on the size of the aneurysm:
- Small aneurysms (less than 4 cm):
Typically monitored with ultrasound every 1 – 2 years. - Medium aneurysms (4 – 5.4 cm):
Typically monitored every 6 – 12 months or more frequently depending on the doctor’s recommendation.
Medication/Drugs
While medications cannot repair an aneurysm, they can manage associated risk factors. Common medications prescribed include:
- Blood pressure medications:
Antihypertensive medications, particularly Beta-blockers or ACE inhibitors, can be prescribed to lower blood pressure and relieve stress on the aneurysm. This reduces the risk of aneurysm growth or rupture. - Cholesterol-lowering medications:
Statins can be used to manage cholesterol levels and prevent atherosclerosis, which can exacerbate aneurysms. - Aspirin:
Low doses of aspirin may be recommended to reduce the risk of blood clots, which can be a complication of aneurysms.

| Medication Class | Mechanism of Action | Side Effects | Brand Names in India |
|---|---|---|---|
| Beta-blockers (or) Antiarrhythmics (Lowers blood pressure) | Reduce heart rate, blood pressure, and heart workload by blocking the effects of adrenaline on beta receptors. | Fatigue Dizziness Bradycardia Depression Cold extremities Erectile dysfunction | (Atenolol) Aten, Betacard, Ziblock (Bisoprolol) Concor, Bisolol |
| ACE Inhibitors (Angiotensin-Converting Enzyme Inhibitors) (or) Vasodilators (Lowers blood pressure, prevents heart attack & helps in heart failure) | Relax blood vessels by blocking the production of angiotensin II, a hormone that narrows blood vessels. | Cough High potassium levels Low blood pressure Dizziness Kidney dysfunction | (Enalapril) Envas, Encardil (Ramipril) Ramace, Cardace |
| Statins (Lowers cholesterol) | Lower LDL cholesterol by inhibiting HMG-CoA reductase, an enzyme involved in cholesterol production in the liver. | Muscle pain Liver damage Digestive problems Increased blood sugar levels | (Atorvastatin) Storvas, Atorva, Lipvas (Rosuvastatin) Rosuvas, Crestor, Rosulip |
| Antiplatelet Agents (Treats/prevents heart attack, angina, chest pain & stroke) | Prevent blood clots by inhibiting platelet aggregation. | Increased bleeding Bruising Stomach upset | (Aspirin) Aspirin, Ecosprin, Loprin (Clopidogrel) Clopilet, Preva |
Surgical Treatment
Surgery is considered if the aneurysm is large (generally 5.5 cm or larger) or if it is growing rapidly or causing symptoms. There are two main surgical options:
- Open Surgical Repair: This is the traditional approach where the surgeon opens the abdomen through a large incision to access the aorta and replaces the weakened portion with a synthetic graft. It is a major procedure that requires general anesthesia with a longer recovery time but is effective for long-term repair.
- Endovascular Aneurysm Repair (EVAR): A minimally invasive procedure where a catheter is used to place a stent graft inside the aorta. It is less invasive and usually involves shorter hospital stays and faster recovery compared to open repair.
Lifestyle Changes for Management
While medical treatment is critical, certain lifestyle changes can help manage the condition and may reduce the risk of complications.
- Quit Smoking:
Smoking is a major risk factor for aneurysms. Quitting not only reduces the risk of aneurysm growth but also benefits overall cardiovascular health. - Maintain a Healthy Blood Pressure:
Maintaining a healthy blood pressure is crucial since high blood pressure can contribute to the expansion of an aneurysm. This can be achieved through dietary changes, physical activity, stress management, and medication if necessary. - Adopt a Heart-Healthy Diet:
Eating a heart-healthy diet that is low in saturated fats, trans fats, cholesterol, and sodium can help manage AAA. Adopt a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. - Regular Exercise:
Engaging in moderate-intensity physical activity, like walking, swimming, or biking, can improve cardiovascular health. It’s important to consult a doctor to recommend safe exercises. - Maintain a Healthy Weight:
Being overweight can increase blood pressure and thus the risk of aneurysm growth. Weight management through diet and exercise is advised. - Manage Stress:
Chronic stress can increase blood pressure. Techniques such as yoga, meditation, or deep breathing exercises can be beneficial. - Avoid Heavy Lifting:
Physical exertion that involves heavy lifting can raise blood pressure temporarily, posing risks for individuals with AAA. - Limit Alcohol Consumption:
Excessive alcohol intake can raise blood pressure and should be consumed in moderation. - Regular Medical Check-Ups:
Regular follow-up and imaging tests can help monitor the size of the aneurysm and detect any changes early.
Allopathic Supplements
While supplements should not replace prescribed medication or treatment, the following may be recommended by healthcare providers to improve cardiovascular health. Always consult your doctor before starting any new supplement.
- Omega-3 Fatty Acids: Helps in reducing inflammation and may support overall heart health.
- Potassium (Dietary source includes beans, avocados, peas, potatoes, greens, spinach, broccoli, cabbage, parsley, bananas, oranges, papayas, dried fruits & nuts dates) – Potassium helps in reducing blood pressure.
- Magnesium (Dietary source includes dry nuts like almonds and cashews, seeds like pumpkin and chia, spinach, dark chocolate, yogurt, banana, and black beans) – Low levels are linked to heart diseases, but routine supplementation is not generally recommended.
- Coenzyme Q10 (CoQ10): Occasionally recommended for people taking statins, as it might help with muscle pain related to statin use.
- Vitamin D: In some cases, vitamin D supplementation is considered if levels are low, as it can impact cardiovascular health.
Note: Consult with a healthcare professional before starting any supplement regimen.

Ayurvedic Treatment
In Ayurveda, “Adhogami Dhamnis” are understood as the abdominal aorta and its branches. In Ayurveda, while there is no direct reference to abdominal aortic aneurysm (AAA), the condition can be understood as a disturbance of Vata dosha affecting the blood vessels. Ayurveda emphasizes balancing Vata dosha and reducing Ama (toxins) to strengthen blood vessels, reduce inflammation, and improve circulation. However, it is crucial to combine such therapies with modern medical care for a life-threatening condition like AAA.
Lifestyle and Dietary Recommendations
- Diet: Consume Vata-pacifying foods like warm, cooked meals with healthy fats. Avoid processed foods, excessive caffeine, and alcohol.
- Herbal Remedies: Herbs like amla, garlic, turmeric, tulsi, ginger, and cinnamon may help reduce inflammation, potentially supporting vascular health in conditions like AAA.
- Yoga and Meditation: Practice regularly to manage stress, lower blood pressure, and support cardiovascular health.
Panchakarma Therapies
Rejuvenation therapy in Ayurveda, known as Panchakarma, focuses on achieving harmony between the physical, mental, and spiritual aspects of oneself. It aims to heal the body through purification and detoxification using techniques such as massage, sweating, and fasting.
- Rasayanam (Rejuvenation Therapy): After detoxification, rasayana herbs are used to restore vitality and improve the elasticity of blood vessels.
Virechana (Therapeutic Purgation)
Gentle purging at regular intervals to eliminate accumulated Ama and detoxify the body.
Deepan and Pachana Medications
- Deepan: Stimulates digestive enzymes and enhances metabolism.
- Pachana: Aids in digestion and clears undigested toxins, ensuring better nutrient absorption.
- Basti (Medicated Enema): Effective in balancing Vata dosha and improving overall circulatory health.
Rasayana and Ojaskara Oushadhas
- After detoxification, Rasayana (rejuvenation) therapies restore vitality and enhance immunity.
- Ojaskara medications improve overall energy and joint health and reduce residual symptoms like swelling and fatigue.
These approaches aim to detoxify the body, strengthen tissues, and restore balance, ensuring holistic management.
Note: Ayurvedic treatments are supportive and should not replace allopathic care for AAA, as the condition can lead to life-threatening complications. Always consult both an Ayurvedic practitioner and a vascular specialist for a customized treatment by an Ayurvedic practitioner integrated with modern care for critical conditions.
Ayurvedic Medicines

| Herbal Medication | Description | Brands |
|---|---|---|
| Arjuna (Terminalia arjuna) | Traditionally used for cardiac health, Arjuna is believed to support healthy blood vessels. | Himalaya, Zandu |
| Ashwagandha (Withania Somnifera) | An adaptogen that helps the body manage stress, which can be beneficial in reducing blood pressure – a risk factor for aneurysms. | Baidyanath, Dabur |
| Triphala Amalaki (Indian Gooseberry), Haritaki (Indian Gallnut or Terminalia chebula), & Bibhitaki (Beleric myrobalan or Terminalia bellerica). | Triphala, a blend of 3 fruits is valued in Ayurveda for its detoxifying and anti-inflammatory properties. It supports vascular health in DVT by enhancing circulation, reducing inflammation, and lowering oxidative stress, helping maintain balanced blood flow and healthy vessels. | Organic India Triphala, Himalaya Triphala |
| Guggulu (Commiphora mukul) | Guggulu is used for lowering cholesterol and managing obesity, which can contribute to heart disease. | Himalaya Shuddha Guggulu |
| Turmeric (Curcuma longa) | Turmeric is known for its anti-inflammatory and antioxidant properties due to its active compound, curcumin. It is traditionally used to reduce inflammation and may help improve circulation. Turmeric can have mild blood-thinning effects, so medical supervision is advised. | Himalayan Organics Curcumin, Appris Herbs Turmeric Haldicurcumin Extract |
| Garlic (Allium sativum) | Garlic is used in Ayurveda for its potential to support heart health and circulation. Like turmeric, garlic also has blood-thinning properties, so it should be used carefully if on blood thinners. | Nature’s Bounty OdorFree Garlic, Garlic Pearls Capsule 100’S |
| Kakubhadi Churna Tablet | It consists of Arjuna bark, Vacha, Rasna herb, Bala, Haritaki, Nagabala, Abhaya, Shati, Pushkarmoola, Pippali, and Sunthil in equal quantity. It is used to treat hypertension and, hence, the risk of AAA. | Kakubhadi Churna Tablet |
| Hridayarnava Rasa Tablets | It consists of Shuddha Parada, Gandhaka, Tamra Bhasma, Kakamachi, and Trikut (Haritaki, Vibhitaki, Amalaki). It helps improve cardiovascular health, thereby helping AAA. This tablet contains metallic ingredients; hence, it should only be taken under strict Ayurvedic supervision. | Baidyanath Hridayarnava Ras |
Siddha Treatment
In Siddha medicine, while there is no direct mention of abdominal aortic aneurysm (AAA), it can be understood as a condition involving impaired circulation and vascular weakness, often attributed to imbalances in “Vatham dosham.” Siddha treatment focuses on strengthening blood vessels, detoxifying the body, and balancing doshas to support vascular health. These therapies are complementary and should be combined with modern medical care for life-threatening conditions like AAA.
Detoxification/ “Kazhichal maruthuvam” (Purgation Therapy)
Kazhichal is a procedure in Siddha medicine used to eliminate vitiated kutrams (imbalanced bodily humors) through the anal route, typically involving purgative therapies to cleanse the system and restore balance. Mild purgatives are used to eliminate toxins and balance or neutralize Vatham. Common forms of purgative medicines include Thailam (medicated oil), Mooligai Podi (herbal powder), Kudineer (herbal decoction), and Mathirai (tablet forms).
- Nervalam (Croton Tiglium):
Nervalam, the seed of the Purgative Croton plant, is a natural laxative used by ancient Siddhars. It is known for its ability to remove Vata dosha and cleanse the intestines. - Kadukkai (Terminalia Chebula):
A common herb used for cleansing and improving digestion. - Vathanaasa Thylam (15 – 30 ml):
Medicated oil taken once daily on an empty stomach in the early morning for 1 – 3 days to help cleanse the system and restore balance. - Rasa Thylam (15 – 30 ml):
This is a type of polyherbal oil used for purgation. Take 15 – 30 ml once daily (OD) for 1 – 3 days. - Sivathai (Operculina Turpethum L. S. Manso) Kudineer:
Also known as the transparent wood rose, it is a “Kudineer” or herbal decoction widely used for purgation but also has antioxidative & anti-inflammatory properties.
Vamana Maruthuvam (Therapeutic emesis)
It is a therapeutic vomiting performed when vitiated Kapha dosha is present in patients, causing excess mucus. Expelling Kapha from the body helps cure the disease and enhances digestion and metabolism.
- Marukkarai Kudineer:
15 – 30 ml, once daily, in the morning on an empty stomach. - Kuppaimeni Saaru:
5 – 10 ml, once daily, in the morning on an empty stomach.
Dietary Recommendations
- Foods that promote warmth and hydration, such as cooked and easily digestible vegetables, whole grains, and healthy fats, are recommended to balance Vatha.
- Include warm soups, stews, ghee, nuts, avocado, coconut, coconut oil, buttermilk, cheese, eggs, whole milk, wheat, and moist foods like melons, zucchini, and yogurt.
- Garlic & pomegranate are believed to help cardiovascular health.
- Include warm spices like ginger, garlic, and turmeric.
- Sweet foods in moderation are key for a Vata-pacifying diet.
- Avoid cold, dry, processed, or refrigerated foods that can aggravate dosha imbalances. This includes cold and carbonated drinks, raw or uncooked fruits and vegetables, frozen items, and leftovers stored in the refrigerator.
- Regular exercise and stress management through meditation and yoga are encouraged.
Lifestyle and Physical Practices
- Yoga and Varma Therapy:
- Varmam is a Siddha therapy involving the stimulation of energy points at nerve, muscle, blood vessels, and tendon junctions. Finger pressure and massage release pranic energy, aiding pain relief and stress and promoting circulation, flexibility, and overall well-being. Type of Varmam used:
- Komberi kaalam
- Vilangu varmam
- Kondaikoli varmam
- Chunnambu kaalam
- Thivalaikaalam
- Veeradangal
- Regular exercise and stress management through meditation and yoga are encouraged.
- Varmam is a Siddha therapy involving the stimulation of energy points at nerve, muscle, blood vessels, and tendon junctions. Finger pressure and massage release pranic energy, aiding pain relief and stress and promoting circulation, flexibility, and overall well-being. Type of Varmam used:
- Oil Massages (Thokkanam): Thokkanam comes from the words Thokku (skin) and Anam (support, tone, or heat). It refers to therapeutic body manipulation, typically performed by hand, using nine techniques. This practice may involve medicated oils and is often paired with internal medicines for enhanced effectiveness. It improves blood flow, strengthens vessel walls, and helps with pain.
- Poochu (Liquid/Oil Poultice): A therapeutic application of oils to soothe and treat affected areas to reduce pain & enhance blood circulation. Common oils used include:
- Mezhugu Thylam
- Saaranai Kalli Thylam
- Ulunthu Thylam
- Vathakaesari Thylam
| Medication | Purpose |
|---|---|
| Venthamarai kudineer/Choornam | Herbal powder that helps one to get rid of issues like depression, hypertension, anxiety, panic attacks and helps to relax nervous system, Choornam Dosage: 1 – 2 gm with lukewarm water, twice daily (BD), after food. Kudineer Dosage: 60 – 80 ml, twice daily (BD), after food |
Note: Please consult a qualified Siddha practitioner and a medical doctor for personalized diagnosis and treatment plans. The information in this table is only for educational purposes and not a substitute for professional medical advice.
Yoga
Yoga can be a beneficial complementary practice advocated by both Ayurvedic and Siddha treatments for individuals dealing with aneurysms, as it helps promote overall well-being, reduces stress, and improves circulation. However, it is essential to consult with a healthcare professional before starting any yoga practice to ensure it is safe for your specific condition. Here are some gentle yoga asanas that might be beneficial:
Pavanamuktasana (Wind-Relieving Pose)
- Improving digestion and alleviating discomfort caused by gas
- Strengthens the abdominal muscles and massages the internal organs
- Promotes overall digestion, relieves tension, and can aid in reducing lower back pain

Vajirasana (Thunderbolt or Diamond Pose)
- Decreases blood pressure and heart rate
- Helps in managing symptoms of type 2 diabetes

Uttanapadasana (The raised leg pose)
- It helps in strengthening the core, which can provide support to the abdominal region, potentially reducing pressure on the aorta.
- This pose encourages better blood circulation, particularly to the lower limbs, which can support overall cardiovascular health.

Ardha Salabhasana (Half Locust Pose)
- Stimulates the abdominal organs
- Massages the abdominal and pelvic organs
- It may restrict breathing; therefore, it may not be suitable for seniors or pregnant women

Sarvangasana (Shoulder Stand)
- Enhances blood circulation by reversing blood flow, benefiting overall vascular health.
- Strengthens the neck, shoulders, and core muscles.
- Stimulates the thyroid and parathyroid glands, supporting hormonal balance.
- Precautions: Avoid if you have neck injuries, severe hypertension, or cardiovascular conditions.

Viparita Karani (Legs-Up-the-Wall Pose)
- Enhances blood circulation, especially in the lower body.
- Relieves tired legs and feet while reducing swelling.
- Improves digestion and stimulates abdominal organs.
- Aids in gentle detoxification by improving lymphatic drainage.
- Precaution: Avoid this pose if you have glaucoma, severe back or neck problems, advanced cardiovascular conditions, or are pregnant or diagnosed with an abdominal aneurysm—consult a doctor beforehand.

Natarajasana (Dancer Pose)
- It strengthens core and lower body muscles, potentially easing strain on blood vessels.
- It promotes balance, flexibility, and improved circulation.
- It must be practiced under medical guidance.

Shavasana (Corpse Pose)
- It promotes deep relaxation, reduces stress, and lowers blood pressure, which can improve aneurysms.
- It helps calm the nervous system, improving overall circulation and reducing strain on blood vessels.
- Regular practice under medical advice can aid in managing the aneurysm safely.

Remember, always practice yoga under the guidance of a certified instructor and ensure that the postures don’t strain your body, especially when dealing with specific health conditions such as an aneurysm.
References:
https://www.mayoclinic.org/diseases-conditions/thoracic-aortic-aneurysm/symptoms-causes/syc-20350188#:~:text=Tears%20in%20the%20wall%20of,may%20be%20difficult%20to%20speak.
https://my.clevelandclinic.org/health/diseases/7153-abdominal-aortic-aneurysm
https://pmc.ncbi.nlm.nih.gov/articles/PMC5595553/
https://www.ncbi.nlm.nih.gov/books/NBK470237/
http://www.rasamruta.com/pdf/113.pdf
https://jaims.in/jaims/article/view/2707/3831
https://pmc.ncbi.nlm.nih.gov/articles/PMC8340719/
https://namayush.gov.in/sites/all/themes/webcms/images/org_str/SiddhaStandardTreatmentGuidelines.pdf
https://namayush.gov.in/sites/all/themes/webcms/images/org_str/SiddhaStandardTreatmentGuidelines.pdf
https://nischennai.org/main/wp-content/uploads/2023/02/e-Book-NIS.pdf
https://www.1mg.com/
OpenAI. (2024). ChatGPT [Large language model]. https://chatgpt.com
