Deep Vein Thrombosis (DVT)
Deep vein thrombosis (DVT) is a blood clot in deep veins, commonly in the legs. It affects 1-2 per 1,000 annually, with higher risk in older adults, women on hormonal therapy, and the obese. Untreated, DVT can lead to pulmonary embolism, with a 15% mortality risk. Prompt treatment ensures good outcomes.
Overview
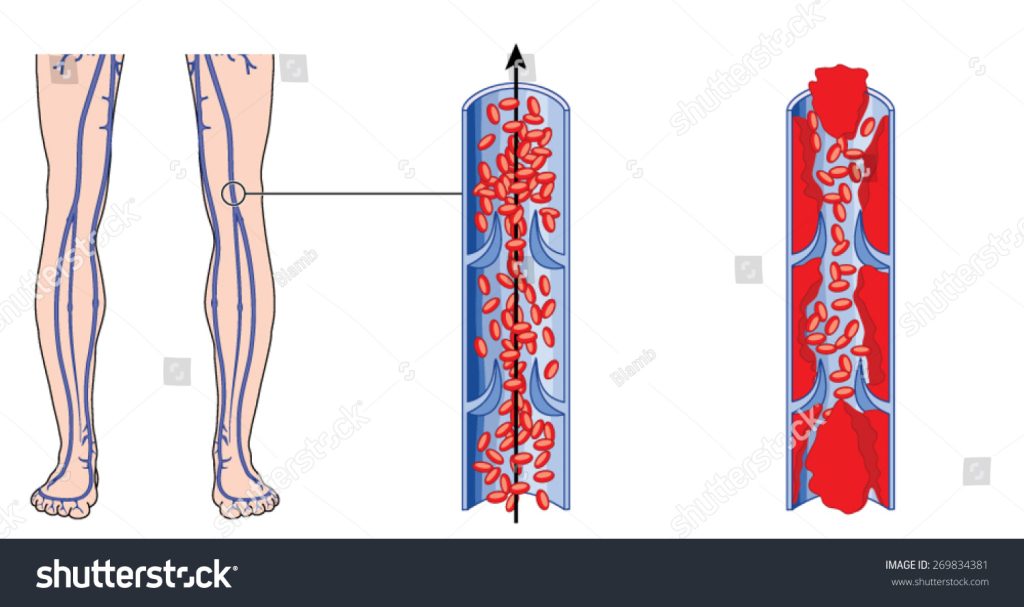
Deep Vein Thrombosis (DVT) is a medical condition that occurs when a blood clot forms in a deep vein, typically in the legs, though it can also occur in other parts of the body. The deep veins in the body are located deeper in the tissue and have a protective function, facilitating the flow of blood back to the heart. DVT develops when blood flow decreases and becomes stagnant, leading to the formation of a clot. DVT can cause leg pain or swelling, but it may also occur without noticeable symptoms.
Types of DVT
| Type | Description | Prognosis | Symptoms |
|---|---|---|---|
| Acute DVT | A clot that occurs suddenly can create an emergency, as DVT is dangerous; pieces of the clot may break off, travel to the lungs, and cause a life-threatening pulmonary embolism (PE). | Depends on timely location, diagnosis and treatment. Cases of PE can be life threatening with advanced age & other health conditions. | Throbbing pain in the affected area Swelling in one leg (rarely in both legs) Warmth in the affected area Red or darkened skin around the painful area—this may be less visible on brown or black skin Swollen veins that are hard or sore to touch Breathlessness in case of PE |
| Chronic DVT | A clot that gradually forms and is older than one to two months is considered “chronic” and hardens over time, scarring and narrowing the vein, which restricts blood flow. | Chronic DVT may cause long-term issues like post-thrombotic syndrome, with pain, swelling, and mobility challenges. While full recovery is tough, consistent management can improve symptoms and quality of life. | Sometimes Asymptomatic Persistent leg pain and swelling Heaviness or aching in the affected limb Skin discoloration (often reddish or brownish) Thickened or hardened skin Varicose veins Ulcers or open sores in severe cases |
Classification of Deep Vein Thrombosis (DVT) based on other factors:
| Type | Description | Prognosis | Symptoms |
|---|---|---|---|
| Provoked DVT | Occurs due to a known risk factor or trigger (e.g., surgery, trauma, immobility). Risk factors may be temporary or long-term. | Good prognosis if the risk factor is addressed. Recurrence may be low if transient risk factors are controlled. | Pain or tenderness in the affected leg. Swelling in the leg, ankle, or foot. Warmth over the clot area. Change in skin color (redness). |
| Unprovoked DVT | Occurs without any apparent triggering event or known risk factor. May suggest an underlying hypercoagulable condition or cancer. | Higher risk of recurrence due to unknown risk factors. Long-term anticoagulation may be necessary. | Leg pain and tenderness, often without a precipitating event. Persistent swelling or edema in the affected leg. Discoloration or erythema over the thrombotic area. Gradual onset of symptoms, which may become more noticeable with time. |
| Proximal DVT | Occurs in the veins above the knee, such as the iliac, femoral, or popliteal veins. It is considered more serious than distal DVT due to the higher risk of pulmonary embolism. | Higher risk of pulmonary embolism. Requires prompt treatment. With proper anticoagulation, prognosis is generally good. | Swelling in the affected leg Pain or tenderness in the leg, often starting in the calf Warmth in the affected area Increased pain when bending the foot Skin discoloration or redness |
| Distal (Calf) DVT | Occurs in the deep veins below the knee, such as the posterior tibial or peroneal veins. It is generally considered less severe due to a lower risk of embolism. | Lower risk of pulmonary embolism compared to proximal DVT. May resolve with or without treatment, but should be monitored. | Mild swelling in the calf Achiness or tenderness in the calf Pain in the calf, especially when walking or standing Possible warmth in the area |
| Upper Extremity DVT | Occurs in the veins of the arms, such as the subclavian or axillary veins. Less common than lower extremity DVT. | Lower risk compared to lower extremity DVT. Can lead to complications if left untreated, but generally good prognosis with treatment. | Swelling in the arm or hand Pain or tenderness in the affected limb Warmth and redness Possible visible veins around the shoulder or neck |
When to See a Doctor for DVT
An untreated DVT can cause several complications such as:
Pulmonary Embolism (PE):
Life-threatening condition where the clot travels to the lungs, causing blockage.
Post-Thrombotic Syndrome (PTS) Or Chronic Venous Insufficiency (CVI):
Chronic pain, swelling, and skin changes in the affected leg due to vein damage. Impaired blood return from the leg, leading to swelling and heaviness.
Recurrent DVT:
Higher risk of new clot formation.
Venous Ulcers:
Persistent sores around the ankles from prolonged vein pressure.
Venous Gangrene (Rare):
Severe tissue death due to blood flow obstruction.
Emergency Situations
While DVT itself isn’t life-threatening, a clot can dislodge and lead to a pulmonary embolism (PE), a dangerous condition where clots block lung vessels and require immediate treatment. Seek urgent medical help if you experience any of the following symptoms, as they may signal a PE:
- Sudden shortness of breath
- Chest pain that worsens with deep breathing or coughing
- Lightheadedness, dizziness, or fainting
- Rapid pulse
- Coughing up blood
Routines for Pre-existing Conditions
If you have DVT or a history of it, regular follow-ups with your healthcare provider are essential. You should:
- See your primary care physician or a specialist, like a hematologist or vascular specialist, every 3 to 6 months (or as advised) to monitor your condition and adjust treatment as needed.
- Follow your prescribed treatment plan, which may include anticoagulants, lifestyle changes, and monitoring for side effects.
Your doctor may suggest more frequent visits if:
- Your condition is unstable or requires close monitoring.
- There are significant changes in your health or medications.
Visits may become less frequent once your condition is stable and well-managed.
Preventative Checkups Based on Family History or Lifestyle Factors
If you have a family history of DVT or risk factors like prolonged immobility, smoking, hormonal therapy use, or a personal history of blood clots, regular checkups with your healthcare provider are recommended. These may be scheduled annually or as advised, based on your risk assessment.
Doctors to Consult
If you are dealing with DVT or concerns about risk factors, consult with the following healthcare professionals:
- General Physician (GP): They can provide initial assessments, referrals, and manage overall care.
- Vascular Specialist: A doctor specializing in blood vessel disorders. They may offer a more in-depth examination and targeted treatments.
- Hematologist: If there is a concern regarding blood clotting disorders, a hematologist can be consulted for specialized care and testing.
Ensuring regular follow-ups with these healthcare providers can help manage and mitigate the risks associated with DVT.
Risk Factors/Causes
Family History & Genetics
- Family history of DVT or pulmonary embolism
- Genetic clotting disorders (e.g., Factor V Leiden mutation, Prothrombin gene mutation)
- Deficiencies in proteins that help prevent clotting (e.g., Protein C, Protein S, Antithrombin III deficiencies)
Age & Sex
- Increasing age (higher risk with advancing age)
- Sex
- Hormonal factors in women including pregnancy and the postpartum period can increase risk for DVT
- Males may have a slightly higher risk compared to females in certain age groups
Lifestyle Habits
- Health related immobility (e.g., Post surgery, confined to bed, disability)
- Sitting still for prolonged periods (e.g., long flights or car rides >3 hours, desk job )
- Smoking
- Obesity
- Sedentary lifestyle
Pre-existing Medical Conditions
- Cancer and cancer treatments (e.g. Chemotherapy)
- Heart disease and related conditions
- Previous history of DVT or pulmonary embolism
- Surgery, especially pelvic, abdominal, or orthopedic surgery
- Injury or trauma
- Chronic medical illnesses such as Inflammatory bowel disease (e.g., Crohn’s disease, ulcerative colitis)
- Varicose veins
- Autoimmune disorders
- Extended use of Hormonal therapy (e.g., birth control pills, hormone replacement therapy)
Prevention of DVT
- Stay Active:
Regular physical activity can help improve blood circulation. Aim to walk or exercise regularly. - Maintain a Healthy Weight:
Being overweight increases the risk of developing DVT. Try to maintain a healthy weight through a balanced diet and regular exercise. - Avoid Prolonged Immobility:
If you’re sitting or lying down for long periods, such as during a long flight or car trip, try to stand up, stretch, and walk around whenever possible. - Exercise your legs when sitting:
If moving around is not an option, perform simple leg exercises like flexing & stretching your feet or rotating your ankles regularly to encourage circulation. - Wear Compression Stockings:
These can help prevent swelling and reduce the chance of blood clots forming, especially if you’re at higher risk for DVT. - Stay Hydrated:
Drink plenty of fluids to stay well-hydrated, as dehydration can increase the risk of blood clots. - Avoid Smoking:
Smoking affects blood circulation and can increase the risk of clot formation. Consider quitting smoking to reduce the risk of DVT. - Follow Medical Advice:
If you’re prescribed blood thinners or other medications to prevent DVT, take them as directed by your healthcare provider. - Elevate Your Legs:
When sitting or lying down, try to elevate your legs to promote blood flow back to the heart. - Manage Other Health Conditions:
Keep chronic conditions like diabetes, hypertension, and high cholesterol under control, as they can contribute to the risk of DVT. - Consider Anticoagulant Medications:
Under the advice of a healthcare provider, blood-thinning medications might be prescribed, particularly after surgery or in high-risk individuals. - Be Mindful of Hormonal Treatments:
If you are using birth control pills or hormone replacement therapy, discuss with your doctor about potential risks and alternatives. - Consult Your Doctor:
Especially if you have risk factors for DVT, consult your healthcare provider for personalized preventive advice. - Follow Post-Operative Guidelines:
After surgery, adhere to recommended practices such as early mobilization and use of any prescribed medications to minimize clot risks.
Diagnosis
Diagnosing Deep Vein Thrombosis (DVT) involves a combination of clinical evaluation, imaging tests, and laboratory assessments. The standard approach follows a series of steps to ensure accurate diagnosis:

Medical History and Physical Examination
The diagnostic process begins with a thorough medical history and physical examination.
- Medical History: Reviewing the patient’s history, including recent surgeries, trauma, immobilization, and known risk factors for thrombosis.
- Physical Examination: Examining the affected limb for signs such as swelling, tenderness, warmth, and redness.
- Well’s Criteria: A clinical scoring system used to assess the probability of DVT based on clinical factors.
Laboratory Tests and Results Interpretation
Following the initial clinical evaluation, laboratory tests may be ordered to aid in the diagnostic process:
- D-dimer Test: A blood test used to detect the presence of a protein fragment from the breakdown of a blood clot. A negative D-dimer test can help rule out DVT in patients with a low to moderate pre-test probability.
Note: Blood thinners can cause a false negative D-dimer test, indicating no clotting disorder when one may exist. Be sure to inform your doctor about any medications you’re taking.
- Coagulation Studies: Tests like Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT) may be conducted to evaluate blood clotting function. Prothrombin time is usually monitored as an international normalized ratio (INR) if you’re taking the blood thinner warfarin.
Note: If you are taking anticoagulant meds then these values will be slightly higher. In which case, please check with your doctor for acceptable therapeutic values.
- Complete Blood Count (CBC): Conducted to rule out other conditions and to assess overall health.
| Lab Test | Optimal | Acceptable | Borderline | High | Critical |
|---|---|---|---|---|---|
| D-dimer Test | <0.5 μg/mL | 0.5 – 1.0 μg/mL | N/A | Greater than 1.0 μg/mL | Significantly elevated levels |
| Prothrombin Time (PT) | 10 – 13.5 seconds | 13 – 15 seconds | 15 – 18 seconds | 18 – 20 seconds | Greater than 25 seconds |
| Activated Partial Thromboplastin Time (aPTT) | 25 – 35 seconds | N/A | 35 – 45 seconds | 45 – 70 seconds | Greater than 70 seconds |
| International Normalized Ratio (INR) | 0.8 – 1.1 | 1.2 – 1.5 | 1.5 – 2.0 | 2.0 – 3.0 | Greater than 3.0 |
| Factor V Leiden Mutation | Normal (no mutation) | N/A | N/A | Heterozygous mutation | Homozygous mutation |
| Protein C and S Levels | 70 – 130 IU/dL mean (range) | 40 – 70 IU/dL mean (range) | N/A | 30 – 40 IU/dL mean (range) | < 30 IU/dL mean (range) |
Imaging Tests
- Compression Ultrasound:
The primary imaging modality used to diagnose DVT. It evaluates blood flow and the presence of clots in the veins of the leg. - Venography:
Also called venogram, is an invasive X-ray procedure that visualizes blood flow in veins to diagnose and manage conditions like blood clots. Although it’s the gold standard, it’s less commonly used due to its invasiveness and potential complications. - CT Venography (CTV):
Uses CT imaging and contrast dye to detect clots, often used when pulmonary embolism(PE) is suspected. - Magnetic Resonance Venography (MRV):
This specialized MRI is used when ultrasound results are inconclusive or when detailed vein visualization is needed. It focuses on the veins without displaying surrounding tissues and usually requires a contrast injection for enhanced visibility. Mostly done when DVT is suspected in the abdominal area.
Follow-up and Additional Testing
After the initial diagnosis, further tests may be performed to investigate underlying causes, especially in patients with recurrent DVT or those under 50 without clear risk factors:
- Coagulation Profile:
Tests for inherited thrombophilias, such as Factor V Leiden, Protein C and S deficiencies, Antithrombin III deficiency, and Prothrombin G20210A mutation, especially if a genetic predisposition to clotting is suspected.
Factor V Leiden and PT 20210 are inherited mutations that increase the risk of excessive clotting. Passed in an autosomal dominant manner, individuals may inherit one mutated gene (heterozygous) or two (homozygous), affecting the severity of their condition. - Antiphospholipid Antibodies:
Tests for lupus anticoagulant and anticardiolipin antibodies, used when antiphospholipid syndrome is suspected. - Further Imaging:
To determine the extent of thrombosis or assess for complications like pulmonary embolism.
A systematic approach to DVT diagnosis is essential for accurate identification and effective management, with clinical assessment and diagnostic tools working together for optimal treatment planning.
Allopathic Treatment
DVT management and treatment focus on preventing clot progression, reducing symptoms, preventing clots from breaking loose, and traveling to the lungs, which can lead to a pulmonary embolism. Key components include:
Allopathic Medications / Anticoagulation Therapy
The cornerstone of DVT treatment in allopathy is the use of anticoagulants, also known as blood thinners, to prevent further clotting.
- Heparin This fast-acting drug is typically administered intravenously in a hospital setting. Low molecular weight heparin can also be given via subcutaneous injection.
- Warfarin An oral anticoagulant typically used for long-term treatment. Regular blood monitoring (INR) is required to ensure the correct dosage.
- Direct Oral Anticoagulants (DOACs), drugs such as rivaroxaban, apixaban, and dabigatran have become popular choices for long-term DVT management due to their fixed dosing and no need for regular INR monitoring.
Please see the allopathic medication section below for details.
| Medication/Drug | Class | Mechanism of Action | Side Effects | Brand Names in India |
|---|---|---|---|---|
| Heparin | Anticoagulant- Unfractionated Heparins (UFH) | Heparin enhances the activity of antithrombin III, which inhibits clotting enzymes thrombin and factor Xa, preventing new clots forming and existing clots from growing. | Bleeding, Thrombocytopenia Osteoporosis (with long-term use), Hypersensitivity reactions | Heparin, Hepaglan, Caprin Hep Lock |
| Warfarin | Anticoagulant/ Vitamin K Antagonist | Warfarin works by blocking vitamin K, which is needed to make certain clotting proteins. This slows down the blood’s ability to form clots, helping to prevent new clots and keep existing ones from growing. | Bleeding, Teratogenic potential, Skin necrosis, Interactions with food and drugs | Warf, Sofarin, Cofarin |
| Enoxaparin | Anticoagulant/ Low Molecular Weight Heparin (LMWH) | Enoxaparin, a low molecular weight heparin, binds to and enhances the activity of antithrombin III, with a stronger effect on factor Xa than on thrombin. This prevents clots from growing and helps reduce the formation of new clots. Given as a subcutaneous injection, often used in hospital settings or for short-term use. | Bleeding, Thrombocytopenia, Injection site reactions | Lonopin, Clexane, Cutenox |
| Rivaroxaban | Direct Oral Anticoagulant (DOAC) – Factor Xa Inhibitors | Rivaroxaban selectively inhibits factor Xa, preventing thrombin formation and thrombus development. Taken orally. | Bleeding, Liver enzyme abnormalities, Allergic reactions | Xarelto, Rivaflo, Rivaxab |
| Apixaban | Direct Oral Anticoagulant (DOAC) – Factor Xa Inhibitors | Apixaban blocks factor Xa, an enzyme needed for clotting, preventing new clots and stopping existing ones from growing. | Bleeding, Anemia, Nausea | Eliquis, Apigat, Cadiquis |
| Dabigatran | Anticoagulant (DOAC) – Direct Thrombin Inhibitors | Dabigatran is a direct inhibitor of thrombin, preventing conversion of fibrinogen to fibrin. | Bleeding, Gastrointestinal symptoms, Hypersensitivity | Pradaxa, Dabigat, Dabifib, Dabitra |
| Fondaparinux | Synthetic Factor Xa Inhibitor | Fondaparinux selectively binds to antithrombin III, enhancing its ability to inhibit factor Xa. | Bleeding Anemia Thrombocytopenia | Arixtra, Fondared, Fondum |
Note: These medicines should always be taken only after consulting your doctor.
Medical Procedures
Thrombolytic Therapy
In cases where the DVT is extensive or life-threatening, thrombolytic agents, also known as clot busters, may be employed to dissolve the clot.
- This treatment is often reserved for severe cases due to the increased risk of bleeding, especially intracranial hemorrhage.
- Catheter-directed thrombolysis: In cases of severe DVT, clot-dissolving drugs are delivered directly to the clot via a catheter to dissolve it, usually reserved for extensive or life-threatening clots.
Inferior Vena Cava (IVC) Filter Placement
An IVC filter may be placed in patients who cannot take anticoagulants. It catches large clots that break off and prevents them from traveling to the lungs, reducing the risk of pulmonary embolism.

Compression Therapy
Compression therapy is commonly used in the management of Deep Vein Thrombosis (DVT) to improve blood flow, reduce swelling, and prevent complications. It helps in blood circulation, reduces swelling & pain and prevents post thrombotic syndrome(PTS)

- Compression Stockings: Recommended to alleviate swelling, improve blood flow, and reduce the risk of post-thrombotic syndrome, these should be worn consistently.
- Compression Wraps and Bandages: These are applied for more severe cases or when stockings are difficult to wear. Wraps can be adjusted to provide the needed pressure.
- Intermittent Pneumatic Compression Devices: These devices use an air pump and inflatable sleeves that wrap around the legs, periodically inflating to provide graduated compression.
Minimally Invasive Procedures
- Endovenous Laser Ablation (EVLA): A minimally invasive procedure that uses laser energy to seal off affected veins contributing to deep vein thrombosis (DVT).

- Radiofrequency Ablation (RFA): Utilizes radiofrequency energy to heat and close veins responsible for DVT symptoms.

- VenaSeal Closure System: Employs medical adhesive to seal damaged veins, redirecting blood flow through healthier veins.
- Ambulatory Phlebectomy: A minimally invasive surgical technique for removing varicose veins through small incisions, often recommended for varicose veins associated with DVT.

Surgical Thrombectomy
In certain cases where anticoagulation and thrombolysis are ineffective, surgical removal of the clot may be necessary, typically for extensive clots that threaten limb viability.
Regular Monitoring and Follow-Up
- Blood Tests: For patients on warfarin, regular INR tests ensure therapeutic levels. For DOACs, routine blood tests are less frequent.
- Clinical Monitoring: Regular check-ups help assess clot resolution, side effects, and overall health, adapting treatment as needed.
Lifestyle Changes for Management

- Regular Exercise: Engage in regular physical activity to improve blood circulation. Activities like walking, swimming, and cycling are beneficial. Exercise also helps in maintaining a healthy weight, which reduces the risk of DVT.
- Weight Management: Maintain a healthy weight through a balanced diet and regular exercise. Excess weight can put pressure on the veins, increasing the risk of DVT.
- Stay Hydrated: Drink plenty of fluids to keep the blood from thickening, which can help prevent clots from forming. Aim for at least 8-10 glasses of water per day, unless advised otherwise by a healthcare provider.
- Avoid Prolonged Inactivity: If you have to sit for long periods, such as during travel or work, make sure to take breaks and move around at regular intervals. Stand, stretch, and walk every 1-2 hours to promote circulation.
- Compression Stockings: Use compression stockings if recommended by your doctor. These can help prevent blood from pooling in the legs and reduce swelling.
- Elevate Legs: Elevate your legs when sitting or lying down to help improve blood flow back to the heart.
- Avoid Smoking: Quit smoking, as it can damage blood vessels and increase the risk of clot formation. Seek support for smoking cessation if necessary.
- Limit Alcohol Consumption: Consume alcohol in moderation as excessive drinking can affect blood clotting.
- Healthy Diet: Consume a diet rich in fruits, vegetables, whole grains, and lean proteins to support overall cardiovascular health. Reducing salt intake can also help manage blood pressure.
Allopathic Supplements
Alongside anticoagulants, some allopathic supplements may support blood flow and vascular health in DVT patients but should only be used under medical guidance due to potential interactions. Common options include:
- Omega-3s:
May reduce clot formation and improve blood flow. - Vitamin E:
Mild anticoagulant; use cautiously with blood thinners. - Garlic Extract:
Enhances circulation but may thin blood. - Curcumin (Turmeric):
Anti-inflammatory; mildly anticoagulant. - Ginkgo Biloba:
Supports circulation, but interacts with anticoagulants. - Magnesium:
May prevent vessel constriction. - Vitamin K Antagonists:
Helps regulate Vitamin K levels involved in blood clotting and can aid in DVT when prescribed by the doctors
Note: Always consult a doctor before making any significant lifestyle changes or starting new medications or supplements to avoid interactions.
Ayurvedic Treatment for DVT
Ayurveda can help manage DVT naturally by enhancing circulation, reducing inflammation, balancing the doshas—Vata, Pitta, and Kapham and dissolving blood clots through a holistic approach encompassing lifestyle modifications, dietary recommendations, herbal medications, and detox therapies.
Note: Ayurveda and Siddha may complement DVT management after the acute phase by supporting blood flow, reducing inflammation, and preventing recurrence. They can also help manage side effects and improve vascular health through diet, lifestyle, and stress reduction. Always consult healthcare providers to safely integrate these with conventional care.
- Dietary Modifications:
Focus on a diet rich in anti-inflammatory foods like fresh fruits, vegetables, whole grains, nuts, and seeds. Limit fatty, oily, and processed foods, and avoid excessive salt and red meat. - Lifestyle Changes:
Regular physical activity and yoga can help improve blood circulation. Avoid prolonged sitting and standing. - Panchakarma Therapy:
Ayurvedic detoxification techniques that may include procedures like Virechana (purgation) and Vasti (enema) to cleanse the body and balance the doshas.- Virechana (Purgation Therapy):
Virechana is a detoxifying therapy that helps cleanse the body of toxins, which can contribute to poor circulation and inflammation. By reducing excess Pitta dosha, Virechana promotes improved blood flow, lowering the risk of blood clot formation and supporting overall circulatory health. - Basti (Enema Therapy):
Basti is one of the cleansing treatments that focus particularly on the colon, using herbal oils to rebalance the imbalance of Vata dosha. Improving circulation along with the removal of impurities decreases the possibility of clot formation in deep veins, proving integral in managing DVT.
- Virechana (Purgation Therapy):
- Herbal Medicines:
Use of specific Ayurvedic herbs and formulations aimed at reducing inflammation, thinning the blood, and promoting circulation. - Abhyanga (Oil Massage):
Abhyanga is an external, oil-based massage therapy that invigorates the body’s circulation, causing blood to flow better and be thicker so clots cannot easily form. It also helps in detoxification, decreases edema in DVTs, and makes one’s vascular function better in general.
Ayurvedic Medicines

| Herbal Medication | Description | Brands |
|---|---|---|
| Brahmi (Bacopa monnieri) | Brahmi supports blood circulation, reduces stress, and improves vascular function, making it beneficial for DVT prevention with its anti-inflammatory and antioxidant properties. | Organic India Brahmi, Kerala Ayurveda Brahmi |
| Guggulu (Commiphora mukul) | Guggul is an anti-inflammatory Ayurvedic herb that improves blood flow, reduces blood viscosity, and supports vascular health, making it effective for DVT management. It also helps lower cholesterol and prevent clot formation. | Himalaya Shuddha Guggulu |
| Arjuna (Terminalia arjuna) | Arjuna is an Ayurvedic herb with cardiovascular benefits, strengthening blood vessels, improving circulation, and reducing clot formation, aiding in DVT management | Jiva Arjuna, Himalaya Arjuna |
| Dashamoola (Ten-Root Compound) | Dashamoola is a powerful blend of ten roots that reduces inflammation, relieves pain, and improves circulation, making it effective for managing DVT. | Baidyanath Asli Ayurved Dashmularishta – 680 ml |
| Sahacharadi Kwath | Sahacharadi Kwath is a traditional Ayurvedic decoction designed to address Vata imbalances, including venous insufficiency and circulation concerns like DVT. Formulated with herbs such as Sahachara, it delivers anti-inflammatory and pain-relieving effects, supporting the health of veins and arteries. | Kerala Ayurveda Sahacharadi Kwath 200 Ml |
| Triphala – Amalaki (Indian Gooseberry), Haritaki (Indian Gallnut or Terminalia chebula), & Bibhitaki (Beleric myrobalan or Terminalia bellerica). | Triphala, a blend of 3 fruits is valued in Ayurveda for its detoxifying and anti-inflammatory properties. It supports vascular health in DVT by enhancing circulation, reducing inflammation, and lowering oxidative stress, helping maintain balanced blood flow and healthy vessels. | Organic India Triphala, Himalaya Triphala |
| Ashwagandha (Withania Somnifera) | Ashwagandha, an adaptogenic herb, reduces stress, promotes relaxation, and supports vascular health, making it beneficial for DVT prevention. | Himalaya Ashvagandha Kapiva Ashwagandha Gold Capsules |
| Punarnava (Boerhavia diffusa) | Punarnava is an Ayurvedic herb known for its diuretic and anti-inflammatory properties, helping to reduce edema and improve circulation by balancing Kapha dosha, improving circulation, supporting blood flow and managing Kapha imbalance associated with DVT. | Zandu Punarnava Capsules, Himalaya Punarnava Tablets |
| Lashunadi Vati | Lashunadi Vati, an Ayurvedic garlic(Lashun) based formulation, supports DVT treatment by improving circulation, reducing clot risk, and managing inflammation, promoting vascular and cardiovascular health. | Dabur Lasunadi Vati, Unjha Lashunadi Vati |
| Kanchnar Guggulu | Kanchnar Guggulu is a polyherbal, Ayurvedic remedy used in DVT treatment to reduce inflammation, improve circulation, and support lymphatic drainage. It helps decrease swelling and promotes vascular health, which can lower blood clot risk. Key ingredients include: Kanchnar (Bauhinia variegata) Guggulu (Commiphora mukul) Trikatu (Black pepper, Long pepper, Ginger) Triphala (Amalaki, Bibhitaki, Haritaki) | Dhootapapeshwar Kanchanar Guggul, Baidyanath Kanchanar Guggulu |
Note: It is essential to consult qualified practitioners before using these medicines, as individual treatment options may vary. Severe conditions may need immediate allopathic care.
Siddha Treatment for DVT
In Siddha medicine, DVT is often associated with imbalances in the body’s fundamental elements(Vatham, Pitham, and Kapham) and humors. The treatment approach focuses on restoring balance through herbal medications, dietary modifications, lifestyle changes and specific therapies. Approaches may focus on reducing inflammation, improving circulation, and purifying blood. However, it is crucial to consult with a Siddha practitioner and a conventional healthcare provider for appropriate diagnosis and treatment.
| Medication | Purpose |
|---|---|
| Cira Turai chooranam | Known for enhancing circulation and reducing inflammation, potentially supporting vascular health in DVT. |
| Ayakantha Chenduram | Used for its blood-purifying and anti-inflammatory properties, which can aid in maintaining healthy blood flow. |
| Seenthil Chooranam | Traditionally used for its immune-boosting and anti-inflammatory effects, which may support vascular health. |
| Pungu Thailam | Often used as an external application to improve circulation. |
| Nilavembu Kudineer | A herbal decoction believed to help in detoxifying and purifying the blood. |
| Thootha Ilai Chooranam | Used for its properties that support healthy blood vessel functioning. |
| Inji (Ginger) Extract | Known for stimulating circulation and reducing swelling. |
| Karuppu Manjal (Black Turmeric) | Contains anti-inflammatory compounds that can help reduce blood vessel inflammation and support circulation. |
Note: It is essential to consult qualified practitioners before using these medicines, as individual treatment options may vary. Severe conditions may need immediate allopathic care. Deep vein thrombosis is a serious condition, and timely western medical intervention can be life-saving.
Yoga
Practicing yoga regularly can potentially support cardiovascular health and improve blood circulation.
Paschimottanasana (Seated Forward Bend)
Benefits: Gently stretches the legs, improving blood flow.

Uttanasana (Standing Forward Bend)
Benefits: Stretches the hamstrings and calves, encourages blood circulation, and calms the mind.

Vajrasana (Thunderbolt Pose)
Benefits: Enhances blood flow in the lower body and aids digestion, which can be beneficial for overall circulatory health.

Tadasana (Mountain Pose)
- Improves posture and balance.
- Increases awareness and focus, aiding in mental calmness.
- Enhances circulation and can help reduce blood pressure.

Vrikshasana (Tree Pose)
- Improves balance and stability in the legs.
- Promotes mental focus and concentration.
- Strengthens the heart by improving overall circulation.

Setu Bandhasana (Bridge Pose)
- Opens the chest, improving heart and lung functioning.
- Reduces anxiety, stress, and tension.
- Improves blood circulation and helps maintain healthy blood pressure.

Viparita Karani (Legs Up the Wall Pose)
Benefits: This pose helps improve blood circulation, reduce swelling in the legs, and relieve stress in the leg veins.

Pavanamuktasana (Wind-Relieving Pose)
Benefits: Aids in digestion and relieves tension in the lower back, promoting circulatory health in the legs and abdomen.

Shavasana (Corpse Pose)
- Promotes deep relaxation and stress relief.
- Calms the mind and reduces anxiety.
- Improves circulation and encourages a healthy heart rate.

