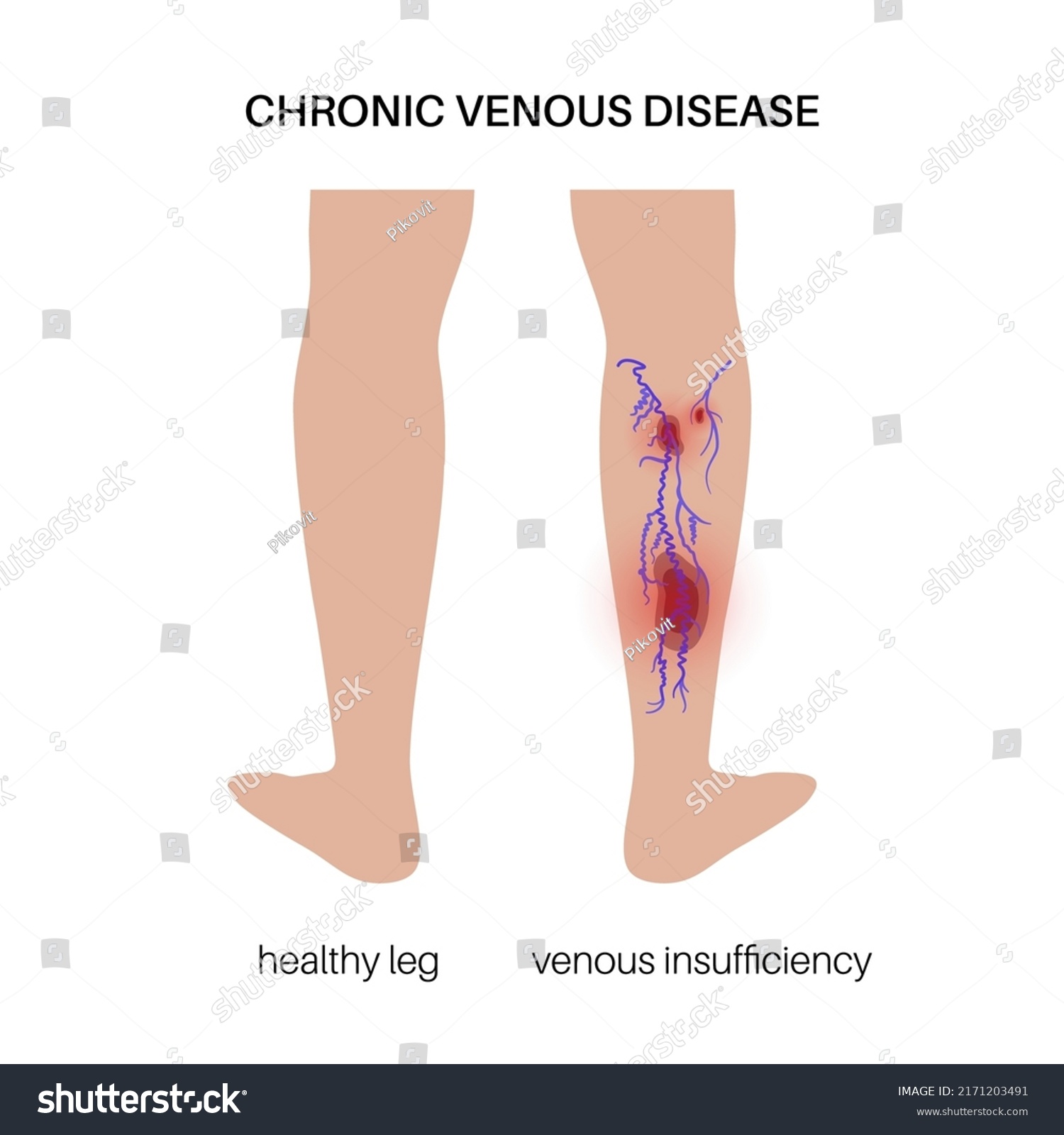
Chronic Venous Insufficiency
Chronic venous insufficiency (CVI) is a common condition, especially in women and people over 50. It happens when the veins in your legs don’t work as they should, which can cause varicose veins, skin ulcers, and other problems if left untreated. While it can affect your quality of life, it’s rarely life-threatening. The good news is that early diagnosis and treatment, like wearing compression stockings or, in some cases, having surgery, can help manage the condition and prevent complications.
Overview
Chronic Venous Insufficiency (CVI) is a medical condition in which the veins in the legs are unable to efficiently return blood back from the leg to the heart. This condition occurs when the vein walls weaken, and valves in the veins become damaged or dysfunctional, which normally prevent blood from flowing backward. Poor blood flow in the legs can cause blood pooling, heaviness, and increased venous pressure. Old age, obesity, history of atrial fibrillation, and myocardial infarction are significant risk factors for CVI. Severe cases may lead to ulcers and skin damage.
Classification of Chronic Venous Insufficiency
Chronic venous insufficiency (CVI) is generally classified based on the causes, location, and blood flow problems. Understanding these classifications helps guide diagnosis, treatment planning, and patient management. All types of Chronic Venous insufficiency have one or more of the following common symptoms:



- Swelling in the legs or ankles
- Varicose veins
- A tight feeling in the calves or itchy, painful legs
- Pain while walking that improves with rest
- Brown discoloration of the skin, usually near the ankles
- Leg ulcers that may be difficult to treat
- A restless sensation in the legs with an urge to move them
- Painful leg cramps or muscle spasms
Types Based on Cause:
CVI is classified by its causes to pinpoint the underlying issue, guide treatment, predict disease progression, and identify potential complications. This approach facilitates targeted treatments, helps achieve better outcomes, and provides patients with a clearer understanding of their condition.
| Type | Description | Prognosis | Symptoms |
|---|---|---|---|
| Primary CVI | Primary chronic venous insufficiency occurs due to inherent weakness or dysfunction of the vein valves, often without underlying conditions. It could be linked to genetic predisposition or prolonged standing. This leads to blood pooling in the veins. | With early detection and management, symptoms can be alleviated, and complications like ulcers may be avoided. Lifestyle modifications and compression therapy are often effective. | Swelling Pain Skin discoloration Varicose veins Leg heaviness |
| Secondary CVI | Secondary chronic venous insufficiency occurs as a result of external factors, such as deep vein thrombosis (DVT), post-traumatic thrombosis/scarring from DVT, external compression (e.g., May-Thurner syndrome, tumors), trauma, or obstruction. This leads to improper blood flow and valve dysfunction. Proper treatment of the underlying cause is crucial to managing symptoms. | Depends on the severity of the underlying cause. Long-term management, including anticoagulants and sometimes surgical interventions, may be necessary to prevent complications. | Persistent swelling Skin discoloration Leg pain Venous ulcers |
| Congenital CVI | Congenital chronic venous insufficiency(CVI) arises from inherited or developmental abnormalities in the venous system, present from birth. Key features include: Venous malformations: Includes Structural abnormalities of the veins (e.g., Klippel-Trénaunay Syndrome) or abnormal connections between arteries and veins (e.g., Arteriovenous fistulas) causing increased venous pressure and dysfunction. Absence or hypoplasia of venous valves: In rare cases, veins lack functional valves or have underdeveloped (hypoplastic) valves, leading to reflux and blood pooling in the lower extremities. | Variable prognosis; early intervention can improve quality of life. Severe cases may require surgical correction or specialized treatments. | Visible vein deformities, Chronic swelling, Skin changes may be seen early in life |
| Functional CVI | It is caused by external factors rather than structural vein abnormalities. Key features include prolonged standing or sitting (leading to impaired blood flow), obesity (increased abdominal pressure), and pregnancy can exacerbate the condition (hormonal changes and uterine pressure affecting venous drainage). | Functional CVI may improve with lifestyle changes, increased mobility, and the use of compression therapy. If managed properly, it rarely leads to long-term complications. However, without intervention, it can worsen, potentially causing chronic symptoms or contributing to more severe venous issues. | Temporary swelling and discomfort that is relieved by movement or elevation, Restlessness in leg, Leg Fatigue or heaviness, particularly towards the end of the day |
Where Can CVI Affect?
Understanding the classification of Chronic Venous Insufficiency (CVI) based on location helps healthcare providers deliver targeted treatments by focusing on the specific venous system involved. CVI results from damage or obstruction of veins or their valves, either directly or indirectly.
- Superficial Venous Insufficiency:
Involves superficial veins, such as the great saphenous vein (GSV), small saphenous vein (SSV), and their tributaries. - Deep Venous Insufficiency:
Affects deep veins, including the anterior tibial, posterior tibial, peroneal, popliteal, deep femoral, superficial femoral, and iliac veins. - Perforator Venous Insufficiency:
Involves perforator veins, which connect superficial and deep veins. These “communicating veins” are primarily located in the thigh and leg. - Mixed Venous Insufficiency:
A combination of superficial, deep, and/or perforator vein involvement. - Pelvic Venous Insufficiency:
Affects veins in the pelvis, such as the ovarian veins or internal iliac veins. It is commonly associated with pelvic congestion syndrome or pregnancy-related venous changes.
What kind of blood flow problems can CVI cause?
- Reflux (Venous Valvular Incompetence):
Backward flow (retrograde flow) due to failure of venous valves to close properly. - Obstruction:
Impeded forward flow due to narrowing or blockage in the veins. - Mixed Reflux and Obstruction:
Combination of backward flow (reflux) and reduced forward flow (obstruction). - Muscle Pump Dysfunction:
Ineffective upward propulsion of blood due to impaired calf muscle pump function, which is usually caused by neurological disorders, reduced mobility & muscle atrophy/weakness.
When to See a Doctor
Chronic Venous Insufficiency, as the name indicates, is often chronic but, when detected early, can be managed with lifestyle changes. However, certain cases require professional medical attention. While mild cases of CVI can often be managed with self-care measures, there are certain indicators that suggest it’s time to seek medical assistance. Consulting a physician for a proper diagnosis and treatment plan is recommended if you are experiencing any symptoms or if you are experiencing other changes in the health of your leg. If untreated, it can lead to potential complications like Venous Ulcers, Pulmonary Embolism (a blood clot breaks free and travels to the lungs), or severe underlying issues.

Emergency Situations
Seek emergency medical help if you experience any of the following with Chronic Venous Insufficiency (CVI):
- A sudden increase in leg pain or swelling.
- Signs of infection in a leg ulcer, such as redness, warmth, pus, or fever.
- New pain, redness, or tenderness along a vein may indicate deep vein thrombosis (DVT).
- Symptoms of a pulmonary embolism (a life-threatening complication) such as chest pain, shortness of breath, rapid heartbeat, or coughing up blood.
- Signs of a blood clot, including redness, warmth, and tenderness over a vein.
Prompt medical attention is essential to prevent serious complications.
Managing Pre-existing Conditions
IIf you have Chronic Venous Insufficiency (CVI) or related conditions, follow these steps:
- Regularly visit your healthcare provider, such as a vascular specialist or phlebologist, for evaluation and management.
- Schedule check-ups every 6–12 months to monitor symptoms and adjust treatment as needed.
- For complications like Deep Vein Thrombosis (DVT), venous ulcers, or pulmonary embolism (PE), more frequent visits may be necessary based on your specialist’s advice.
- Plan an annual consultation with a vascular specialist to monitor and manage associated venous conditions effectively.
Preventative Checkups Based on Family History or Lifestyle Factors
By prioritizing early detection, risk assessment, and lifestyle changes, individuals can improve their quality of life and reduce the risk of severe CVI complications. Preventative steps include:
- Start with an initial assessment by a general physician.
- Schedule check-ups with a vascular specialist every 1–2 years, even if you have no symptoms.
- Maintain a healthy lifestyle with regular exercise, weight management, and avoiding smoking.
- Visit your general physician annually to address health concerns, especially if there’s a family history or lifestyle-related risks.
Which Doctors to See
- General Physician: Conducts initial evaluations and manages symptoms, serving as the first point of contact for care.
- Vascular Specialist: Specializes in diagnosing and treating diseases of the vascular system, which includes arteries, veins, and lymphatic vessels throughout the body, excluding the heart and brain.
- Phlebologist: These are doctors who specialize in vein diseases, particularly varicose, spider veins, leg ulcers, and chronic venous insufficiency. They can handle both the medical and aesthetic aspects of venous insufficiency.
- Dermatologist: For skin changes or complications arising from CVI.
Diagnosing the underlying cause assists in determining the proper course of treatment and management needed.
Risk Factors/Causes
Family History & Genetics
- A family history of varicose veins or venous disorders increases the risk.
- Genetic predisposition can affect vein structure, valve function, or collagen production, leading to weakened veins.
Age & Sex
- Age: The risk of developing CVI increases with age due to the natural weakening of vein valves and surrounding muscles over time
- Sex: Women are more prone to developing CVI due to hormonal changes (pregnancy, menopause, contraceptives).
Lifestyle Habits
- Prolonged periods of standing or sitting: Long periods of immobility can hinder blood flow and increase venous pressure, leading to weakened valves over time
- Lack of physical activity: Sedentary lifestyles contribute to weakened muscles that assist in venous blood flow, increasing susceptibility to CVI
- Obesity: Increases pressure on the veins, worsening venous reflux.
- Smoking: Tobacco use harms vascular health by thickening the blood, promoting clot formation, damaging blood vessels, and impairing circulation.
Pre-Existing Medical Conditions:
- Deep Vein Thrombosis (DVT): A history of DVT, where blood clots form in deep veins, can damage vein valves and significantly increase the risk of CVI.
- Obesity: Excess weight adds pressure on leg veins, leading to valve dysfunction and a higher likelihood of CVI.
- Pregnancy: The growing uterus and hormonal changes during pregnancy increase pressure on leg veins and reduce vein elasticity.
- Leg Injury or Trauma: Injuries or surgical procedures can damage vein integrity and function, raising the risk of chronic venous issues.
- Phlebitis: Inflammation of the veins, often in the legs and associated with superficial veins, can contribute to venous insufficiency.
- Heart Disease: Cardiac disorders can impair circulation, increasing venous pressure and reducing blood return to the heart, which worsens leg pooling and leads to valve dysfunction over time.
- Hypertension: Elevated blood pressure increases stress on vein walls, leading to venous dilation, valve dysfunction, and impaired blood flow
- Diabetes: High blood sugar can damage blood vessels, impair circulation, and weaken vein walls, increasing the risk of venous insufficiency and delayed wound healing.
Prevention of Chronic Venous Insufficiency
- Exercise Regularly:
Engage in activities like walking, cycling, or swimming to improve circulation in your legs. - Maintain a Healthy Weight:
Keep your weight in check to reduce pressure on your veins. Obesity strains leg veins, so losing weight can alleviate this and lower CVI risk. - Elevate Your Legs:
Raise your legs above heart level several times a day to enhance blood flow. - Avoid Prolonged Standing or Sitting:
Change positions regularly to prevent increased pressure on your veins. Take breaks to move if you must stand or sit for extended periods. - Wear Compression Stockings:
If advised by your doctor, use compression stockings to prevent blood from pooling in your legs, improve circulation, and reduce swelling. - Eat a Healthy Diet:
Choose foods high in fiber and low in salt to prevent swelling and support vascular health. - Quit Smoking:
Smoking damages blood vessels and impairs circulation, so avoid it to protect vein health. - Avoid Tight Clothing:
Refrain from wearing tight clothing around your waist, legs, or groin to prevent restricting blood flow. - Regular Medical Check-ups:
Visit your healthcare provider for routine check-ups to detect signs of CVI early, especially if you have a family history of the condition. - Practice Good Posture:
Maintain good posture to promote blood flow. Avoid crossing your legs while seated, as it can block circulation and increase vein pressure. - Practice Good Skin Care:
Keep your legs clean and moisturized to prevent infections. - Eat a Healthy Diet:
- Stay Hydrated:
Drink plenty of water throughout the day to maintain healthy circulation and prevent dehydration, which can thicken blood and reduce blood flow. - Include High-Fiber Diet:
- Include fiber-rich foods to prevent constipation, which increases abdominal pressure and affects venous return.
- Sources: Whole grains, fruits (e.g., apples, berries), vegetables (e.g., spinach, broccoli), nuts, and seeds.
- Limit Salt Intake:
Reduce sodium consumption to prevent water retention and swelling in the legs. Opt for low-sodium alternatives and season with herbs or spices instead of salt. - Incorporate Anti-Inflammatory Foods:
- Include foods rich in antioxidants to promote vascular health and reduce inflammation.
- Sources: Berries, pomegranate, turmeric, ginger, dark leafy greens, particularly microgreens, tomatoes, fatty fish (e.g., salmon, mackerel), urad dhal, green tea, and nuts.
- Consume Healthy Fats:
- Choose heart-healthy fats to support overall vascular health, such as unsaturated fats, including monounsaturated and polyunsaturated fats, which are essential for the body. These fats are typically liquid at room temperature and are found in foods like olive oil, canola oil, sesame oil, and sunflower oil.
- Sources: Olive oil, sunflower oil, flax seeds, chia seeds, avocados, eggs, tofu, nuts, olives, dark chocolate, yogurt, nut & seed butter, and fatty fish.
- Increase Vitamin C and Bioflavonoids:
- Support vein strength and repair with vitamin C and bioflavonoid-rich foods.
- Sources: Citrus fruits, jamun, black currant, guava, papaya, kiwi, bell peppers, red chilies, and dark leafy greens.
- Avoid Processed Foods:
Limit processed snacks and fast foods high in sodium and unhealthy fats, as they can contribute to inflammation and poor circulation. - Moderate Caffeine and Alcohol:
Keep caffeine and alcohol intake in moderation to avoid dehydration and circulatory strain.
- Stay Hydrated:
Diagnosis
Chronic Venous Insufficiency (CVI) is diagnosed through a combination of medical history, physical examination, and diagnostic tests. The evaluation process is aimed at determining the extent of venous dysfunction, identifying any complications, and ruling out other possible causes of the symptoms. The following outlines the typical steps and tests involved in diagnosing CVI:
Medical History and Physical Examination
The first step in diagnosing CVI is taking a detailed medical history and performing a physical exam to identify risk factors and conditions like deep vein thrombosis (DVT), a common cause of CVI.
The physician will ask about symptoms like leg pain, swelling, skin changes, or ulcers. The exam includes checking for varicose veins, edema, skin discoloration, and ulcers. They also consider the patient’s occupation, lifestyle, family history, and past vein-related health issues.
CEAP Clinical Score in Diagnosis
Doctors use the CEAP tool to classify Chronic Venous Insufficiency (CVI) based on four key factors: Clinical, Etiological, Anatomical, and Pathophysiological. Before CEAP, diagnosing chronic venous disorders was unclear, leading to errors in studies and treatments. The CEAP system standardized the diagnosis, improving communication among healthcare professionals and allowing for more accurate diagnoses and better management of the condition. Here’s how it’s scaled:
| C (Clinical): Evaluates visible symptoms. | C0: No visible signs of vein issues. C1: Small spider veins or tiny varicose veins. C2: Larger varicose veins. C3: Swelling in the legs. C4: Skin changes like discoloration or thickening. C5: Healed venous ulcers (wounds). C6: Active venous ulcers. |
| E (Etiological): Determines the cause of CVI. | Ec: Congenital Ep: Primary Es: Secondary En: No venous etiology identified |
| A (Anatomical): Identifies which veins are affected. | As: Superficial veins Ap: Perforator veins Ad: Deep veins An: No venous location identified |
| P (Pathophysiological): Explains how the veins are malfunctioning | Pr: Reflux P0: Obstruction Pr/o: Reflux and obstruction Pn: No venous pathophysiology identifiable |
How CEAP Works
The CEAP clinical score helps classify the severity of the condition based on visible signs and symptoms on the surface. However, deeper vein issues, which cannot be detected through physical examination alone, often require a venous duplex ultrasound for accurate diagnosis.
This specialized scan examines all the veins in the legs and pelvis to identify hidden problems. Doctors never rely solely on the clinical score to diagnose or treat varicose veins or other vein conditions without performing this essential test.
- Doctors perform a detailed assessment of symptoms, medical history, and vein imaging (e.g., ultrasound).
- Based on findings, each CEAP component is assigned a classification (e.g., C3 for swelling, E primary, A superficial veins, P reflux).
- The complete CEAP score (e.g., C3, Ep, As, Pr) provides a comprehensive understanding of the condition.
Benefits of CEAP
- Helps standardize diagnosis and treatment plans.
- Tracks disease progression over time.
- Guides personalized treatment to improve outcomes.
- Aids in clear communication of symptoms.
Non-Invasive Diagnostic Tests
- Doppler Ultrasound:
Doppler Ultrasound is the most common and important test for diagnosing CVI. It assesses blood flow in the veins and can detect issues like reflux (backward blood flow), blockages, and blood clots. This non-invasive test provides real-time images of the veins.
The procedure takes 30 minutes to 1 hour and involves applying a special gel to your legs and using a handheld device (transducer) that sends sound waves. The device is moved over your skin to capture images and measure blood flow, helping to identify any abnormal flow, such as reflux, which signals valve problems. - PhotoPlethysmography(PPG):
PhotoPlethysmography (PPG) is a non-invasive, painless test that detects blood volume changes in the small veins of the skin. It helps evaluate venous refill time and identify reflux. A small sensor is placed on your lower leg or foot, emitting infrared light to measure blood flow. The test takes 15-30 minutes, and as you move (e.g., standing or raising your legs), it detects any abnormal blood flow, aiding in treatment decisions. - Air Plethysmography (APG):
It is a non-invasive test that measures volume changes in the leg to assess venous function, including reflux, blood flow, obstruction, and calf muscle pump efficiency. It is painless and typically takes 20–30 minutes. Air-filled cuffs are placed around the lower leg, and air is pumped into the cuffs to detect volume changes as blood flows. During the test, you’ll be asked to perform movements like leg raises or foot flexing while the cuffs inflate and deflate. This helps evaluate how effectively your veins fill and empty, aiding in the detection of venous reflux or poor circulation.
Advanced Diagnostic Imaging
- Venography:
Rarely used today, venography is reserved for complex cases or when other imaging methods, like ultrasound, are insufficient. This procedure involves injecting a contrast dye into the veins, allowing them to be visualized on an X-ray. The X-ray usage exposes the patient to radiation. It takes about 30-60 minutes, during which you may feel a warm sensation from the dye. Venography provides detailed images of vein structures and helps identify blockages, blood clots, valve conditions, or other abnormalities. - Magnetic Resonance Venography (MRV):
It is a non-invasive imaging technique that uses MRI technology and magnetic fields to create detailed images of veins and surrounding tissues. It may involve a contrast dye but can sometimes be done without it. The procedure takes 30–90 minutes and involves no radiation exposure. MRV is useful for:- Detecting deep vein issues, structural abnormalities, or blockages contributing to CVI.
- Assessing the severity of venous reflux.
- Guiding treatment decisions, especially for surgical options like endovenous laser therapy or radiofrequency ablation.
- Ambulatory Venous Pressure Measurement:
This minimally invasive procedure measures changes in venous pressure during activity, offering valuable insights into calf muscle pump efficiency and venous reflux. A small catheter is placed in a vein in the foot to directly measure venous pressure and track emptying and refill rates as the patient performs exercises like standing or walking. The test typically takes 30–60 minutes and is considered the gold standard for assessing venous hypertension and the severity of Chronic Venous Insufficiency (CVI).
Common Lab Tests for CVI:
While laboratory tests are not typically used to diagnose CVI directly, they may be prescribed to rule out other conditions or complications. These include:
- D-Dimer Test:
Measures levels of D-dimer, a protein fragment from blood clots. Used to rule out deep vein thrombosis (DVT), a risk factor for CVI. - Complete Blood Count (CBC):
Evaluates red and white blood cells and platelets. Helps assess overall health and identify anemia, infections, or inflammation, particularly in cases involving venous ulcers or skin changes. - Coagulation Studies:
Includes Prothrombin Time (PT) and Partial Thromboplastin Time (PTT). Assesses clotting ability and identifies hypercoagulable states contributing to vein dysfunction. - Blood glucose and lipid profile:
To assess underlying health issues. - Metabolic Panel:
To evaluate kidney and liver function, which can affect fluid balance and venous pressure. - Serum Albumin:
Low albumin levels can indicate poor nutrition or systemic conditions contributing to edema. - Venous Blood Gas (VBG) (rare):
Evaluates oxygenation and CO2 levels in venous blood, sometimes used in advanced cases. - Inflammatory Markers:
Tests like C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) can detect inflammation linked to venous ulcers or complications.
Anti Brachial Index(ABI)
Although the Ankle-Brachial Index (ABI) is primarily used to assess arterial insufficiency, it can help rule out coexisting arterial issues that may impact CVI treatment. This non-invasive test evaluates blood flow and identifies peripheral artery disease (PAD). Blood pressure cuffs are placed on the arms and ankles, and a handheld Doppler device measures arterial flow. The test is painless and takes about 10–15 minutes, and it ensures a comprehensive assessment of venous and arterial conditions contributing to leg symptoms.

Allopathic Treatment
The allopathic treatment approach includes a combination of lifestyle changes, local care, medications, and surgical options to improve venous circulation, alleviate/ manage symptoms, and prevent complications. The following are common strategies utilized in allopathic medicine for treating CVI:
Conservative Treatments
Lifestyle Modifications
- Exercise:
Regular physical activity, particularly walking and stretching your calf and thigh muscles, helps improve leg muscle function and blood flow. - Weight Management:
Maintaining a healthy weight can reduce pressure on veins. - Leg Elevation:
Raising the legs above heart level when sitting or lying down can help reduce swelling. - Adopt a Venous Healthy Diet:
Include foods high in fiber and low in salt to prevent swelling and promote vascular health. - Avoid Tight Clothing:
Steer clear of tight clothes around your waist, legs, and groin, as they can restrict blood flow. - Stay Hydrated:
Drink plenty of water to improve hydration and circulation, reducing the risk of blood clots. - Quit Smoking:
Smoking harms circulation and exacerbates vein problems, so stopping is crucial for better vein health.
Compression Therapy
Compression therapy is a cornerstone treatment for CVI and a conservative approach. It involves the use of medical-grade compression garments or devices (zinc bandages, multiple-layer bandages, etc.) that apply controlled pressure to the legs, helping improve blood flow, reduce swelling, and prevent complications. If ulcers don’t improve with compression, surgery may be necessary.

How Compression Therapy Works
- Enhances venous return by pushing blood back toward the heart.
- Reduces venous pressure and swelling.
- Improves lymphatic drainage and prevents blood pooling.
Types of Compression Therapy
- Compression Stockings:
- Available in knee-high, thigh-high, or pantyhose styles.
- Made with elastic materials to apply graduated pressure (highest at the ankle, decreasing upward).
- Compression Bandages:
- Used for more advanced cases or for patients with venous ulcers.
- Includes short-stretch and multi-layer bandages.
- Intermittent Pneumatic Compression (IPC) Devices:
- Machines with inflatable cuffs that periodically apply pressure to the legs.
- Used in severe cases or when patients cannot tolerate stockings.
- Custom-Fit Compression Garments:
- This is for patients with irregular leg shapes or advanced conditions.
Pressure Levels and Stages of CVI
Compression stockings are classified by their pressure levels, measured in millimeters of mercury (mmHg):
- Mild Compression (8–15 mmHg):
For mild swelling, varicose veins during pregnancy, or prevention. - Moderate Compression (15–20 mmHg):
For mild varicose veins and minor swelling and people at risk of venous insufficiency. - Firm Compression (20–30 mmHg):
For moderate varicose veins, post-surgical recovery, and CVI stages with mild edema. - Extra-Firm Compression (30–40 mmHg):
For severe varicose veins, advanced CVI, and venous ulcers. - Higher Compression (40–50 mmHg or above):
For severe conditions, such as lymphedema or after surgical intervention.
How Long to Wear Compression Therapy
- Daily Use:
Typically worn throughout the day and removed at bedtime. - Ulcers or Severe Edema:
Compression may need to be worn for longer durations under medical guidance. - Long-Term Treatment:
Many patients with CVI require ongoing compression therapy for maintenance.
Key Considerations
- Proper Fit:
Compression garments must be fitted to ensure efficacy and comfort. - Application:
Easier to put on in the morning when legs are less swollen. - Medical Supervision:
It is necessary to determine the right compression level and ensure no contraindications (e.g., severe peripheral arterial disease). - Contraindications:
- Compression therapy should be avoided in patients with severe arterial insufficiency, heart failure, or certain skin conditions without consulting a healthcare provider.
- Poorly fitting stockings may cause discomfort, pressure sores, or worsen ischemia in legs with poor arterial flow.
- Allergies to the material can lead to dermatitis, discoloration, or blistering.
Medication/Drugs
Allopathic medications used for the treatment of Chronic Venous Insufficiency (CVI) primarily focus on managing symptoms, reducing inflammation, improving venous tone, and preventing complications. Venous tone refers to how much the veins resist blood flow and maintain pressure. When the veins tighten (venoconstriction), it increases resistance and pressure, causing more fluid to leak into surrounding tissues. Using a phlebotonic drug to improve venous tone can help manage vein widening (venodilation) that worsens venous insufficiency.
Here’s a list of commonly used medications:
| Medication Class | Mechanism of Action | Side Effects | Brand Names in India |
|---|---|---|---|
| Venoactive Drugs(VAD) (or) Phlebotonics – Gamma-benzopyrones (Natural Flavonoids (aka) Bioflavonoids) (Improves Venous tone & treats CVI symptoms of inflammation, swelling and pain) | Flavonoids, plant-derived compounds, enhance venous tone, reduce capillary permeability, and improve lymphatic drainage. They act as antioxidants, reducing oxidative stress and inflammation while stabilizing vein walls by inhibiting collagen- and elastin-degrading enzymes. Certain combinations, like Rutosides, also aid in pain management alongside treating CVI. | Flavonoids, plant-derived compounds, enhance venous tone, reduce capillary permeability, and improve lymphatic drainage. They act as antioxidants, reducing oxidative stress and inflammation while stabilizing vein walls by inhibiting collagen- and elastin-degrading enzymes. Certain combinations, like Rutosides, also aid in pain management alongside treating CVI. | (Diosmin): Venex, Dosmin, Hesdin (Hesperidin): Biotex Hesperidin, Natural Factors Citrus Bioflavonoids, Forever C Plus NUTRACEUTICAL (Rutosides – Bromelain + Trypsin + Rutoside): Tolpazen, Enzoflam SV, Rutoheal |
| Venoactive Drugs (or) Phlebotonics – Semi-Synthetic and Synthetic Flavonoids (Improves Venous tone & treats CVI symptoms of inflammation, swelling and pain) | Semi-synthetic and synthetic flavonoids are designed to be more effective and durable. They strengthen blood vessels by reducing leakiness and enhancing resilience. They work by preventing white blood cells from becoming overactive, migrating, or adhering to vessel walls. MPFF (Micronized Purified Flavonoid Fraction) lowers harmful molecules like VCAM-1 and ICAM-1, protecting small blood vessels affected by chronic venous insufficiency (CVI). It also improves lymphatic system function, reduces capillary permeability, and shields the microcirculation from inflammation. Calcium dobesilate complements this by reducing blood viscosity and improving overall circulation. | Nausea Diarrhea Abdominal pain Headache Dizziness Rash Itching (pruritus) Fatigue Flu-like symptoms In rare cases: Swelling Difficulty breathing Potential liver enzyme changes (requires monitoring) | (Micronized purified flavonoid fraction Diosmin +Hesperidin): Daflon, Avonoid, Venostor (0-(β-hydroxyethyl)-rutosides (HR) (or Troxerutin) Calcium Dobesilate+Troxerutin): Troxerutin CD, Rutin, Vazocap, Venoruton (Calcium dobesilate): Dobesil, Rutin CD, Dobest (Naftazon (Not available in India, commonly used in Europe)): Mediaven, Etioven, Metorene (Venoruton-Pycnogenol (VE-PY): |
| NonSelective Phosphodiesterase inhibitor (PDEi) (Improves blood flow & tissue perfusion) | Pentoxifylline improves blood flow by reducing blood viscosity, enhancing red blood cell flexibility, and decreasing platelet aggregation. It also widens blood vessels slightly and reduces inflammation, helping manage conditions like chronic venous insufficiency and peripheral vascular disease. It may help reduce improper white blood cell activation and enhance oxygen supply to deprived tissues. | Nausea and vomiting Dizziness or lightheadedness Headache Indigestion or upset stomach Flushing (warmth or redness in the face) In rare cases: Allergic reactions (rash, itching, swelling) Chest pain Irregular heartbeat Bleeding or bruising easily Blurred vision | (Pentoxifylline): Flexital, Flowpent, RB Flex |
| Triterpenoid Saponins (Improves Venous tone & treats CVI symptoms of inflammation, swelling and pain) | Saponins are natural compounds found in plants such as: Escin (from Horse Chestnut Extract – Aesculus hippocastanum) Ruscus Extract (from Butcher’s Broom – Ruscus aculeatus) Escin has been studied for many years and has been shown to reduce inflammation, swelling, and pain. Recent research confirms that escin helps reduce blood vessel leakage in inflamed areas, which helps prevent swelling. Studies on human veins also suggest that escin can strengthen blood vessels. It may protect blood vessels by preventing damage to important molecules, keeping them healthy. Both oral escin tablets and the topical gel are effective for treating injuries and chronic venous insufficiency, and they are generally well-tolerated. The exact way escin reduces swelling and inflammation is not fully known. Note: Avoid raw horse chestnut seeds, as they are toxic unless properly processed. | Upset stomach, nausea, vomiting, and diarrhea. Skin rashes, itching, or more severe reactions in sensitive individuals. Excessive consumption may lead to a drop in blood pressure. In rare cases, saponins can damage red blood cells, leading to hemolysis. High doses may affect liver or kidney function in some rare cases. | Escin (Not available in India): Venastat, Reparil-N gel Veinocap Phyto Capsules (available in India) |
| Anticoagulants or Blood thinners (Dissolves & prevents blood clots) | Anticoagulants, or blood thinners, are used in Chronic Venous Insufficiency (CVI) to manage complications like deep vein thrombosis (DVT) or reduce the risk of venous thromboembolism (VTE). It acts by inhibiting the clotting factors or the platelets. Note: See DVT for more information. | Bleeding risk Drug interactions Thrombocytopenia | (Heparin): Heparin, Hepaglan, Caprin, Hep Lock (Warfarin): Warf, Sofarin, Cofarin (Enoxaparin): Lonopin, Clexane, Cutenox (Rivaroxaban): Xarelto, Rivaflo, Rivaxab (Apixaban): Eliquis, Apigat, Cadiquis (Dabigatran): Pradaxa, Dabigat, Dabifib, Dabitra (Fondaparinux): Arixtra, Fondared, Fondum |
| Antibiotics (Treats infection) | Antibiotics are not a primary treatment for Chronic Venous Insufficiency (CVI) but may be prescribed in cases where complications like infections arise, particularly in the presence of: Infected Venous Ulcers – Common infections involve Staphylococcus aureus or Streptococcus species. Cellulitis – A bacterial skin infection that can develop due to poor circulation and skin breakdown in CVI patients Infected Dermatitis or Eczema – CVI-associated stasis dermatitis may sometimes become secondarily infected. It can be given orally or through IV, depending on the severity of the infection. | (Doxycycline): Doxytop, Doxiguard, Lenteclin (Clarithromycin): Clariwin, Claribid, Crixan (Erythromycin): Erythrocin, Erycin, Eritab | |
| Profibrinolytic & Antithrombotic – Glycosaminoglycan (GAG) / Mesoglycan (Supports blood vessel strength, integrity, and flexibility & treats CVI ulcers) | (Glycosaminoglycans (GAGs) are long, unbranched, sulfated polysaccharides made of repeating disaccharide units. In the body, vascular GAGs are key components of the extracellular matrix (ECM) and endothelial glycocalyx in blood vessels. They are crucial for maintaining vascular integrity, regulating blood flow, and facilitating interactions between cells, signaling molecules, and the ECM. Mesoglycan, a natural GAG, is derived from sources like cow lungs, cow blood vessels (aorta), or pig intestines. Commonly taken as tablets or injections in European countries to treat chronic venous insufficiency (CVI)/ associated leg ulcers, mesoglycan supports blood vessel health by improving blood flow, reducing inflammation and damage, and minimizing capillary leakiness. | Generally safe for oral use, but may occasionally cause: Nausea Vomiting Heartburn Headache Diarrhea Skin reactions | Mesoglycan (Not available in India): Euromedica Mesoglycan, Terry Naturally healthy arteries |
Other Medications
Your doctor may prescribe:
- Diuretics: To reduce swelling by removing excess fluid.
- Antiplatelet Agents: Medications like aspirin may be used to reduce the risk of clots.
- Topical steroid creams: To ease skin inflammation and irritation.
Minimally Invasive Treatment Procedures
For more severe cases or when conservative measures are ineffective, the following procedures might be considered:
Sclerotherapy
Sclerotherapy is a minimally invasive treatment for varicose and spider veins. A saline-based or foam solution is injected into the affected vein, causing it to collapse and be absorbed by the body. This helps redirect blood to healthier veins, improving circulation and reducing symptoms like swelling, pain, and visible veins. Ultrasound may be used for more precise injections.

Endovenous Laser Therapy (EVLT) :
EVLT is a minimally invasive procedure used to treat varicose veins and chronic venous insufficiency (CVI). During the procedure, a laser fiber is inserted into the affected vein through a small incision, usually under ultrasound guidance. The laser emits heat that causes the vein to collapse and seal shut. Over time, the body absorbs the treated vein, and blood is rerouted to healthier veins.
- EVLT typically takes between 30 to 60 minutes.
- Local anesthesia is used so you remain awake and comfortable during the procedure.
- The treated veins may be sore, bruised, or swollen post-treatment, but these symptoms usually resolve within a few weeks.

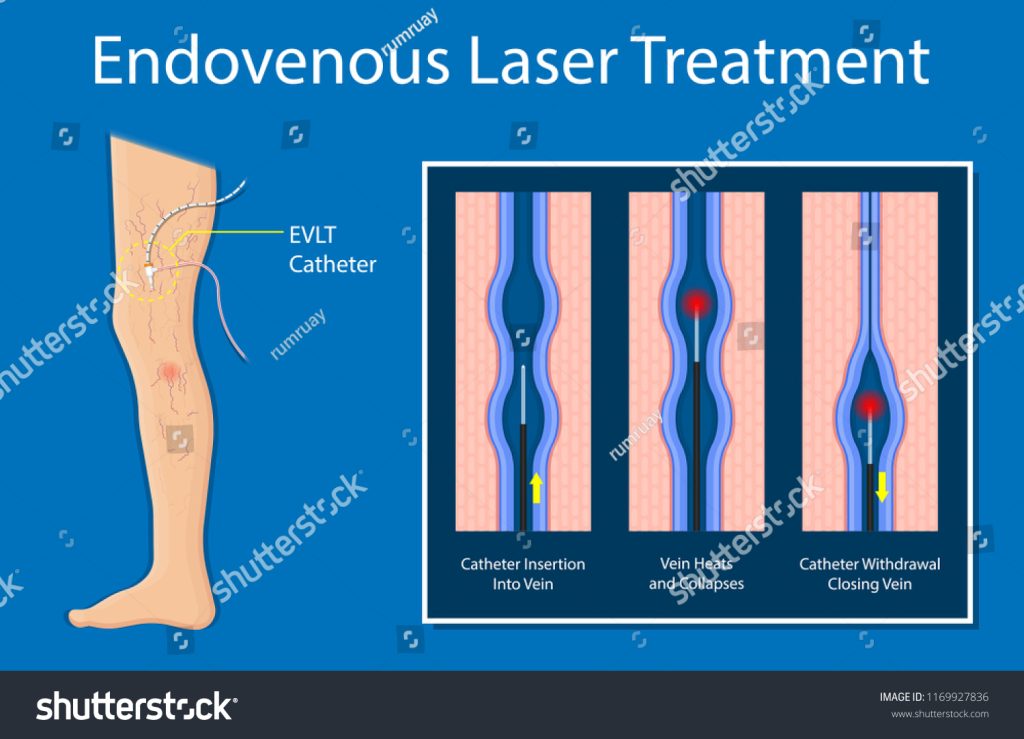
Potential risks include bruising, minor burns, or temporary nerve irritation. Proper post-procedure care, such as wearing compression stockings, enhances recovery and outcomes.
Radiofrequency Ablation (RFA)
RFA is a minimally invasive procedure like EVLT. In this procedure, a catheter with a radiofrequency electrode is inserted into the vein under ultrasound guidance. The electrode uses heat to collapse the vein, which is then absorbed by the body as blood flow is redirected to healthier veins.
Common Guidelines for Sclerotherapy, EVLT & RFA Procedures
Your doctor may recommend some of these based on your condition before performing the procedure.
- Medications to Avoid:
- Antibiotics:
Avoid tetracycline or minocycline 7-10 days before and after to prevent skin staining. - Anti-inflammatory Drugs:
Stop aspirin, ibuprofen, and similar medications 48 hours before and after treatment to prevent interference and excessive bleeding. Acetaminophen is allowed. - Prednisone:
Check with your doctor about stopping prednisone 48 hours prior, as it can reduce the treatment’s effectiveness. - Anticoagulants or Blood thinners:
- Blood thinners may interfere with sclerosing agents, increasing the risk of bruising and bleeding.
- Antibiotics:
- Eligibility:
These are not suitable for those who are pregnant, breastfeeding, bedridden, obese, or within three months postpartum. It is also not recommended for those with active blood clots, DVT, severe arterial disease, recent illnesses, heart conditions, or allergies to the sclerosing solution. - Preparation:
- Do not apply lotion to your legs before or after the procedure.
- Wear or bring shorts/appropriate clothing for the treatment.
- Bring compression stockings to ensure proper fit and support after the procedure.
- Inform your doctor about any allergies, medical conditions, or medications you’re taking.
- Post-Procedure Care:
- Wear compression hosiery or wraps for 3 to 7 days.
- Walk regularly after the procedure to encourage blood flow
- Avoid hot baths, whirlpools, saunas, and strenuous exercise.
- Shower with cooler water.
- Wash the injection sites with mild soap and lukewarm water.
- Avoid applying heat to the treated areas.
- Stay out of direct sunlight, including tanning beds.
- Bruising and discomfort may occur but are typically short-lived.
- These procedures offer significant relief, reducing symptoms and improving the quality of life for patients with chronic venous insufficiency (CVI). These are minimally invasive with a quick recovery.
Note: In most cases, your doctor will avoid performing these procedures on veins that may be needed for future surgical bypass procedures, like the saphenous vein for coronary artery bypass graft surgery, unless the vein is already unsuitable.
Invasive Surgical Procedures
Surgery may be necessary for severe cases of CVI, particularly when other treatments fail, or complications arise and the vein has to be removed. Common surgical options include:
Vein Stripping
- Removal of the main saphenous vein through small incisions.
- Performed in hospitals under general anesthesia.
- Redirects blood flow to healthier veins.
Ambulatory Phlebectomy:
- A newer alternative to vein stripping
- Minimally invasive procedure to remove the affected smaller varicose veins through tiny skin punctures.
- Usually done under local anesthesia.
Please check with your doctor about post-surgical practices.
Regular Monitoring and Follow-up
Regular follow-ups help ensure effective treatment and allow for necessary adjustments. Compression therapy and lifestyle changes are ongoing parts of management. A comprehensive, personalized approach with your healthcare team is key to managing symptoms and improving quality of life.
Allopathic Supplements
In addition to lifestyle modifications, some allopathic supplements may support the management of Chronic Venous Insufficiency (CVI):
- Vitamin E:
Vitamin E is a potent antioxidant with anti-inflammatory properties that help reduce vein inflammation and improve varicose vein health. Vitamin E helps prevent blood clots by reducing platelet clumping. Good sources include nuts and seeds like almonds, pecans, pistachios, walnuts, and sunflower seeds. - Vitamin C:
Vitamin C supports vein health by promoting collagen production and endothelial cell production, as well as protecting nitric oxide. It helps prevent varicose veins and works well when taken with Vitamin E. Citrus fruits are excellent sources. - Vitamin B-Complex:
Vitamin B complex supports vein health by maintaining healthy red blood cells and cholesterol. Vitamin B3 reduces inflammation in vein linings, boosts energy in endothelial cells, and improves blood flow. Vitamins B6, B9 (folate), and B12 lower homocysteine, a molecule linked to blood vessel damage and poor circulation. - Vitamin K:
Vitamin K is essential for healthy blood clotting, as seen when a cut or scrape heals. Unlike older anticoagulant treatments that inhibited vitamin K, newer options are safer. Vitamin K also helps maintain vein health by preventing endothelial dysfunction and increasing nitric oxide levels. Good sources of vitamin K include dark leafy vegetables, animal products, and fermented plant foods. - Copper:
Copper supports circulatory health by aiding red blood cell production and promoting healthy connective tissue in veins. It also helps regulate iron levels, preventing cell damage. Dark chocolate is a great source of copper, along with deep green leafy vegetables, beans, nuts, and seafood. - French maritime pine bark/Pycnogenol:
Pine bark extract, rich in active compounds found in peanut skin, grape seed, and witch hazel bark, boosts collagen production and stabilizes the basal membrane while scavenging free radicals. It reduces capillary leakage, inflammation, and edema with no reported side effects or blood abnormalities. - Grape Seed Extract:
Rich in oligomeric proanthocyanidin complexes (OPCs), which may enhance circulation and reduce swelling in the legs.
Note: Always consult with a doctor before beginning any supplement regimen, especially if you are already taking other medications or have underlying health conditions.
Ayurvedic Treatment
In Ayurveda, CVI is associated with Siraja Granthi, which refers to venous abnormalities characterized by swelling and dysfunction. Ayurveda offers natural ways to manage CVI by improving circulation, reducing inflammation, and balancing Doshas (Vata, Pitta, and Kapha). A holistic approach combines lifestyle changes, dietary recommendations, herbal remedies, and detox therapies to support vein health and alleviate symptoms.
Ayurveda can complement CVI management by supporting blood flow, improving vascular health, detoxifying blood, and preventing recurrence. It may also help reduce the side effects of conventional treatments through personalized diet, stress management, and herbal support. It will not be able to provide a complete cure.
Note: Always consult your doctor before integrating Ayurvedic treatments with conventional care to ensure safety and effectiveness.
Dietary and Lifestyle Recommendations
- Anti-Inflammatory Foods:
Incorporate fresh fruits (e.g., berries, citrus fruits like Amla), vegetables (especially leafy greens), and whole grains (like oats and quinoa) to reduce inflammation and improve circulation. - Fiber Intake:
High-fiber foods are essential to prevent constipation, which can exacerbate CVI symptoms. Include legumes, nuts, seeds, and whole grains in your diet. - Hydration:
Drink plenty of water to help flush out toxins and support overall circulation. - Healthy Fats:
Use healthy fats like ghee and olive oil in cooking, as they can help balance Vata dosha. - Foods to Avoid:
Avoid Processed foods, Salty foods, and Aggravating food types. - BioFlavinoids:
Buckwheat, asparagus, and berries are rich in rutin.
In addition to dietary changes, Ayurveda emphasizes a holistic approach that includes:
- Regular gentle exercise to promote circulation without overexertion.
- Stress management techniques such as meditation or yoga.
- Adequate rest and sleep to support healing processes
Herbal remedies:
- Pineapple Juice:
Rich in bromelain, it helps improve circulation and reduce inflammation, potentially alleviating symptoms of CVI. - Chirabilva Paste:
Applying a paste made from the bark and leaves of Holoptelea integrifolia (Chirabilva) can reduce skin discoloration and improve the appearance of varicose veins. - Pomegranate or Beetroot Juice:
Both are rich in antioxidants and nitrates, which enhance blood flow and vascular health. - Spices:
Incorporating ginger, garlic, and chili into your diet supports circulation by thinning the blood and improving vascular function. - Olive Oil:
Its healthy fats promote blood flow and support overall cardiovascular health when used in cooking. - Fenugreek:
Including fenugreek in your diet helps balance Vata, Pitta, and Kapha doshas, supports healthy blood circulation, strengthens muscles, and reduces inflammation in blood vessels.
These remedies can complement medical treatments but should not replace professional advice for managing CVI. Consult a doctor before starting any new regimen.
Therapies

- Abhyanga:
This Ayurvedic massage technique involves applying warm herb-infused oils to the body, which helps balance the doshas and improves circulation. Oils like Eranda or Castor bean oil, Sesame oil, and Healthvit Veinneed oil can be used for massaging. - Swedana (Hot Fomentation):
In Patrapindasweda, a combination of medicinal herbs such as Eranda (Ricinus communis), Nirgundi (Vitex negundo), and Arka (Calotropis gigantea), among others, is heated in herbal oil in a non-stick pan along with other ingredients. The heated mixture is then wrapped in a clean cloth to form a bolus known as Patra Pinda. This bolus is used to gently rub the body with mild pressure. During the process, it is repeatedly dipped in the warm oil to maintain its temperature. This helps enhance blood circulation, supports the upward flow of blood, and effectively alleviates pain and swelling.
- Panchakarma Therapies:
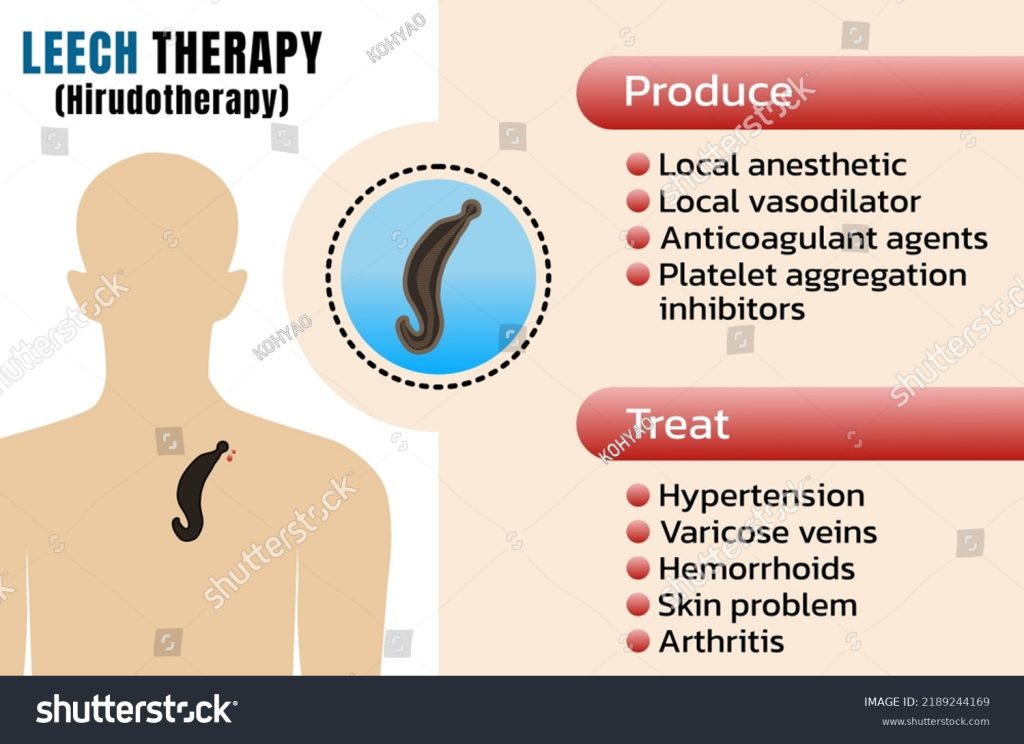
These detoxification procedures, including Raktamokshana (bloodletting), can help improve blood flow in the legs by removing unhealthy blood from the veins.- Jaloukavacharana (Leech Therapy): A bloodletting technique using leeches to enhance blood circulation. Leeches naturally secrete blood-thinning compounds, ensuring steady blood flow in the affected area.
- Siravedhana (Venesection): A bloodletting procedure involving puncturing to remove localized toxins from the blood. It promotes healthy circulation, reduces local pressure and engorgement, and helps maintain the veins’ valve function and elasticity.
- Basti Treatment (Medicated Enema): Involves administering herbal oils into the rectum to reduce inflammation and support overall vascular health
- Avagahana Karma:
This involves immersing the legs in a medicated oil bath, which may help reduce symptoms of chronic venous insufficiency.
Stress Management
- Meditation:
Helps calm the mind, balances Vata, and reduces stress, which can improve circulation. - Dinacharya or Daily Routine:
Establishing a daily routine with early rising (4:30–5:00 am), drinking warm water, regular bowel movements, exercise, meditation, relaxing before bed, and consistent sleep promotes balance and enhances overall health.
Ayurvedic Medicines
| Medication | Description | Brands |
|---|---|---|
| Gotu Kola (Centella asiatica) | It contains triterpenic acid, which helps manage cellulite, venous insufficiency, and varicose veins by stimulating collagen and elastin production to strengthen vein walls. | HealthyHey, Planet Ayurveda, Ayurvedix Organic |
| Guggulu (Commiphora mukul) | Reduces inflammation, purifies blood, enhances blood circulation, and promotes tissue regeneration. | Baidyanath, Dabur, Kerala, Ayurveda |
| Ashwagandha (Withania somnifera) | Strengthens venous valves, decreases swelling and discomfort, enhances circulation, and improves stamina. | Himalaya, Baidyanath, Zandu, HealthyHey |
| Triphala | Detoxifies and balances doshas, aiding in improving circulation and strengthening vein walls | Baidyanath, Dabur, Maharishi Ayurveda |
| Arjuna (Terminalia arjuna) | Supports cardiovascular health, improves vein health, helps in relieving inflammation, and dissolves blood clots. | Himalaya, Baidyanath, Birju Mahavir |
| Brahmi (Bacopa monnieri) | Improves blood flow, maintains healthy blood vessels, prevents blood clotting, and contributes to overall well-being. | Himalaya, HealthyHey, Baidyanath, Kerala Ayurveda |
| Horse Chestnut Extract (Aesculus hippocastanum) | Strengthen vein walls and reduce swelling. Promote normal tone of the vein wall. | Trexgenics, Solaray, Healthvit |
| Manjistha (Rubia cordifolia) | It balances vitiated Pitta dosha, promoting blood purification, improving blood circulation, and alleviating swelling in the legs. | Himalaya Manjistha Tablets, Just Jaivik, HerbtoniQ |
| Butcher’s Broom (Ruscus aculeatus) | Positive effect on blood flow and helps reduce leg swelling | Dr.Bram’s Organic Butcher’s Broom Root Extract Capsules (470 mg) |
| Bilberry | Strengthen blood vessels and capillary walls and improve red blood cells. | HealthyHey Nutrition Natural Bilberry Extract 60 vegetable capsules |
| Bromelain | Promote better circulation and prevent the swelling and soreness caused by varicose veins. | Trexgenics, HealthHey, Healthvit |
| Pine Bark Extract | Reduce leg and ankle edema, makes blood vessels stronger and more elastic, thereby improving circulation | Citrus Nutraceutical, Greendorse, Humming Herbs |
| Sweet Clover (Melilotus officinalis) | Treats blood clots in the veins, supports venous health and eases varicose veins, leg pain and heaviness, phlebitis, and thrombotic conditions. | Mystique Hills Sweet Clover Powder |
| Amalaki (Emblica officinalis) | Amla and other citrus fruits are rich in vitamin C, which is vital for collagen formation in connective tissues. A deficiency in vitamin C is a key factor in the worsening of varicose veins & venous insufficiency | Organic India Amalaki capsules |
| Nirgundi (Vitex negundo) | Reduces inflammation and alleviates pain associated with venous insufficiency. | Herbal Hills, Ayurvedic Life, Way2Life |
| Arogyavardhini Vati | Supports liver function, promotes digestion, reduces swelling, and helps purify blood. | Dabur, Baidyanath |
| Punarnava (Boerhavia diffusa) | Supports kidney function and heart health, cleans and rejuvenates the body, and strengthens the circulatory system. | Herbal Hills, Ayurvedic Life, Way2Health |
| Sariva (Indian Sarsaparilla) or (Hemidesmus indicus) | Sariva root extract purifies the blood, eliminates toxins, and improves circulation. Applied topically, it alleviates varicose vein symptoms such as skin irritation, itching, dryness, dark spots, and uneven skin tone. | Naturmed’s Sariba/Sariva/Indian Sarsaparilla Powder 200mg |
| Chirabilva(Indian Elm Tree)/ Holoptelea Integrifolia Planch | Reduces inflammation blood purification, reduces blood clots, balancing doshas | Planet Ayurveda Chirbilva Churna |
Please consult with a qualified Ayurvedic practitioner for a personalized treatment plan, as these treatments might require customization based on individual health conditions and body constitution (Prakriti). It may be safer to opt for allopathic care for severe conditions.
Siddha Treatment
Siddha medicine, a traditional Indian healing system, offers several natural remedies and lifestyle adjustments for managing chronic venous insufficiency (CVI). While Siddha treatments should be customized based on individual conditions, here are general approaches that may help:
Siddha medicine, a traditional Indian healing system, offers several natural remedies and lifestyle adjustments for managing chronic venous insufficiency (CVI). While Siddha treatments should be customized based on individual conditions, here are general approaches that may help:
Dietary Recommendations
- High Fiber Foods:
A diet rich in fiber is essential as it aids digestion and prevents constipation, which can exacerbate CVI symptoms.- Eat fruits like apples, berries, and citrus fruits.
- Take a lot of leafy green vegetables like kale and spinach.
- Take whole grains, which include Oats, quinoa, and barley.
- Eat Legumes and Nuts like lentils, chia seeds, and walnuts.
- Avoid Cold and Processed Foods:
Cold foods and beverages should be generally avoided. - Vaatham and Pitham Balancing Foods:
A diet that balances Pitham and Vaatham is recommended. Warm, moist, and foods containing healthy fats, such as those with ghee or olive oil, help balance Vaatham. Consuming fiber-rich foods, whole grains, dairy products, and sweet fruits are recommended to counteract the dry and irregular qualities of Vaatham. - Anti-Inflammatory Foods:
Use herbs and spices such as turmeric and ginger to help reduce inflammation and promote better blood circulation. - Avoid Excess Salt:
Reducing sodium intake is crucial as it can lead to fluid retention and exacerbate swelling in the legs. - Foods to Avoid:
Avoid intake of bitter, pungent, astringent, and processed foods.
Lifestyle Modifications and Therapies:
- Avoid Prolonged Sitting or Standing:
Taking breaks to move around can prevent blood from pooling in the legs. - Skin Care:
Regularly moisturizing the skin can help prevent dryness and cracking, which can be exacerbated by CVI. - Footwear Choices:
Opt for low-heeled shoes instead of high heels to promote better blood flow.
Herbal remedies
- External Treatments:
- Padikara Neer: Apply this herbal wish to clean the affected area.
- Ottradam (Fomentation): A therapy using hot or cold packs made from medicinal leaves, pulses, lime, or brick powder applied to the affected area. It reduces swelling, aids in dermatological conditions, and promotes sweating to disperse aggravated doshas and cleanse body channels.
- Kattu (Bandage Dressing): A technique involving the application of herbal or inorganic medicines to the affected area, followed by bandaging. It is used for inflammations and to handle pain.
- Mathan Thailam: This oil is used externally to dress wounds and enhance healing.
- Massage: A few drops of Pungampoo oil with a carrier oil, such as coconut or sesame oil, are mixed and gently massaged onto the affected areas to ease pain and swelling.
Detoxification Techniques:
- Raktamokshana (Bloodletting):
This technique involves the removal of impure blood to improve circulation and alleviate symptoms associated with venous congestion. - Leech Therapy (Attai Vidal):
This traditional treatment involves applying leeches to affected areas, which may help improve blood flow and reduce symptoms associated with varicose veins - Virechana (Induced Purgation):
Virechana is another detoxification method that involves administering herbal formulations to induce purgation. This process helps cleanse the digestive system and eliminate excess bile and toxins from the body, which can contribute to venous disorders. - Basti (Medicated Enema):
Basti therapy involves administering herbal decoctions or oils rectally. This method is particularly effective in balancing Vata dosha and promoting detoxification through the rectal route, facilitating better absorption of nutrients and elimination of waste. - Shuddhi(Detoxification process):
Aims to purify the body and enhance the efficacy of medicinal herbs.
Stress Management:
- Physical Activity:
Regular physical activity is vital for managing CVI symptoms. - Yoga:
Yoga practices specifically designed to enhance circulation can be particularly effective. Poses that promote leg elevation and gentle stretching help improve venous return and alleviate discomfort associated with CVI. - Limit Caffeine and Nicotine:
Both substances can constrict blood vessels and trigger symptoms. Reducing or eliminating caffeine (found in coffee, tea, chocolate, and some medications) and quitting smoking can improve overall vascular health and reduce the frequency of episodes.
Siddha Medications
| Medication | Purpose | Brand Name |
|---|---|---|
| Parangipattai Chooranam | Known for its anti-inflammatory properties, this formulation may help reduce symptoms associated with venous insufficiency. | IMPCOPS Parangipattai Chooranam Tablets, SKM Parangipattai kudineer chooranam |
| Sangu Parpam | Improves blood circulation and reduces swelling. | SKM Siddha and Ayurveda, Impcops Sangu Parpam tablets |
| Silasathu Parpam | Improves blood circulation and reduces swelling. | IMPCOPS Sangu Parpam Tablet, Medisiddh |
| Vallarai Tablet | Used as an antioxidant. | IMPCOPS Vallarai Tablets (Mandukaparni), Kaviraj Siddha Vallarai Capsule |
| Rasa gandhi mezhugu | Balances vata, improves circulation, promotes blood circulation, and reduces inflammation. | SKM Rasagandhi Mezhugu Capsules |
| Seenthil Choornam | Traditionally used for its immune-boosting and anti-inflammatory effects, which may support vascular health. | SKM Seendhil Choornam, Medisiddh Seendhil chooranam |
| Nilavagai Choornam | Alleviates symptoms associated with varicose veins and venous ulcers and reduces symptoms such as swelling, itching, and discoloration of the skin caused by poor venous circulation. | SKM Nilavagai Choornam, IMPCOPS Nilavagai Choornam |
| Thetraivali Rasayanam | Rejuvenates tissues, improves overall vitality, combats oxidative stress, and enhances blood circulation. | Kottakkal Ayurveda, Rasayanam |
| Pungampoo Thailam | Strengthening vein walls, alleviating swelling and discomfort, and supporting overall vascular health. | Dabur, Medisiddh, JRK Siddha Research and Pharmaceuticals |
| Vara Choornam | A herbal formulation that improves venous health, strengthens blood vessels, and purifies the blood. | Vaidyaratnam, Sreedhareeyam Ayurveda, Brahmi Online |
| Amukkara Choornam | A herbal powder, known for improving circulation and reducing stress. Also used to alleviate various ailments, including joint pain, inflammation, and anxiety. | SKM Amukkara Choornam, Aadhavan Amukkara Herbal Capsules |
| Pinda Thailam | Medicated oil used to alleviate pain and burning sensation associated with CVI. Enhances blood flow and supports joint and vascular health. | Arya Vaidya Sala Kottakkal Ayurvedic Pinda Tailam, Kerala Ayurveda Pinda Thailam |
| Vasambu Legium | A herbal jam that aids in improving circulation and reducing venous congestion. |
Note: Please consult a qualified Siddha practitioner and a medical doctor for personalized diagnosis and treatment plans. The information in this table is only for educational purposes and not a substitute for professional medical advice. Severe conditions may require immediate allopathic care.
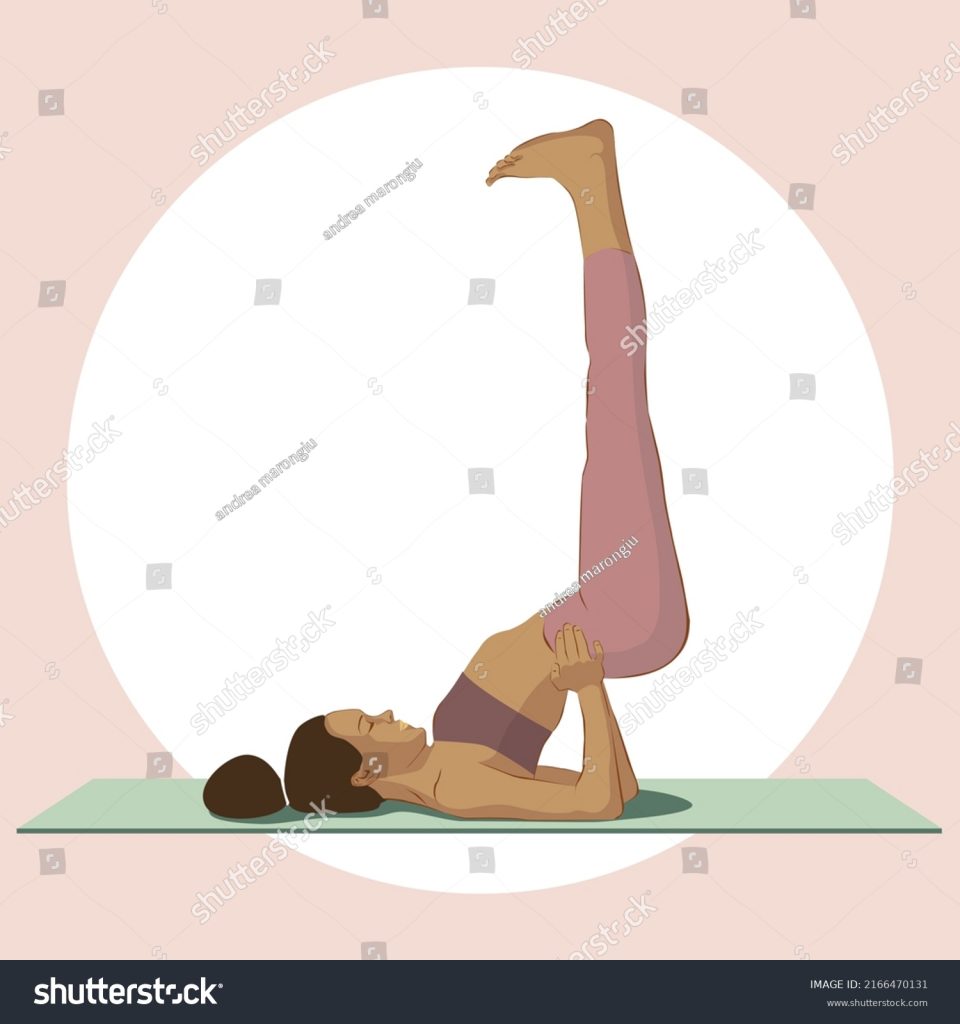
Yoga
Yoga can help manage Chronic Venous Insufficiency by improving circulation, reducing stress, and promoting relaxation. Ayurvedic and Siddha guidelines recommend yoga to enhance blood flow and alleviate symptoms. Yoga can be an effective complementary practice to alleviate some of these symptoms by improving circulation and reducing pressure in the leg.
Viparita Karani (Legs-Up-the-Wall Pose)
- Relaxes the nervous system and provides stress relief.
- Facilitates circulation and alleviates swollen ankles and tired legs.
- Promotes overall relaxation and can help to soothe headaches.
- Helps prevent fatigue and promotes overall well-being.
Tadasana (Mountain Pose)
- Strengthens posture and balance.
- Promotes better blood circulation.
- Reduces stress and promotes relaxation.
- Helps cultivate body awareness and mindfulness of physical sensations.

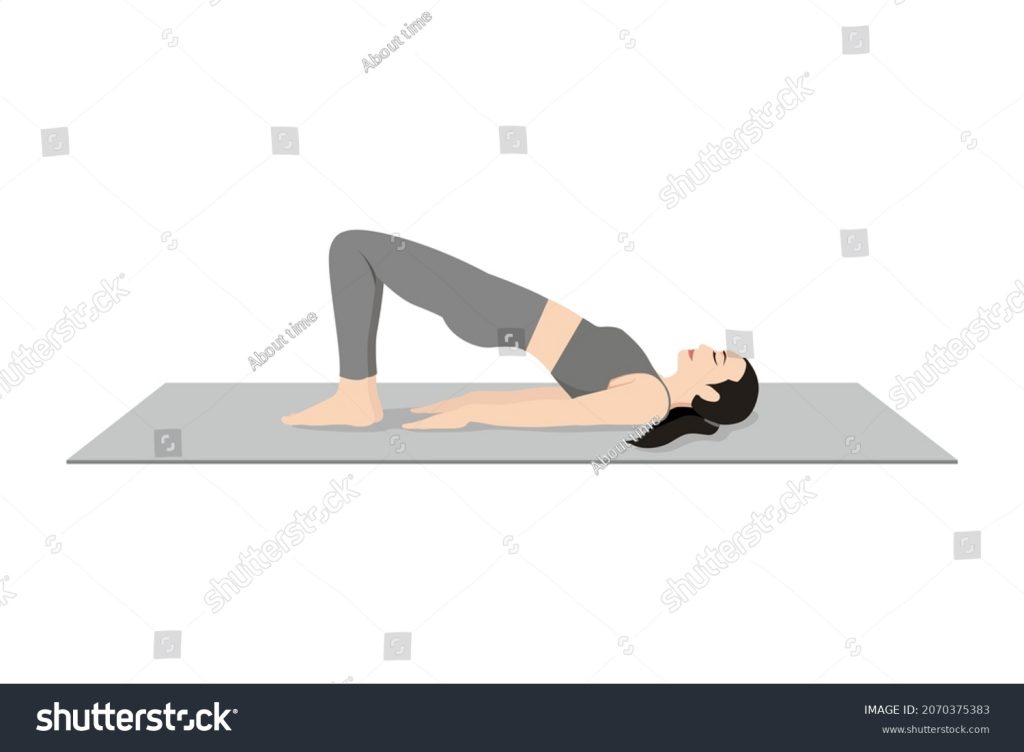
Setu Bandhasana (Bridge Pose)
- Opens the chest and improves lung capacity.
- Stimulates the abdominal organs and improves digestion.
- It can activate the parasympathetic nervous system, which calms the body and reduces stress.
- Strengthens the back muscles while stretching the chest, neck, and spine
Pavanamuktasana (Wind-Relieving Pose)
- Improving digestion and alleviating discomfort caused by gas
- Strengthens the abdominal muscles and massages the internal organs
- Promotes overall digestion, relieves tension, and can aid in reducing lower back pain

Uttanasana (Standing Forward Bend)
- Calms the brain and helps relieve stress.
- Improves digestion and circulation.
- Helps in muscle relaxation, which can alleviate tension that might contribute to vascular constriction.

Adho Mukha Svanasana (Downward-Facing Dog)
- Increases blood circulation to the brain and extremities.
- Strengthens arms, legs, and core muscles.
- Calms the mind and energizes the body.
- Has a calming effect on the nervous system, which can help reduce stress

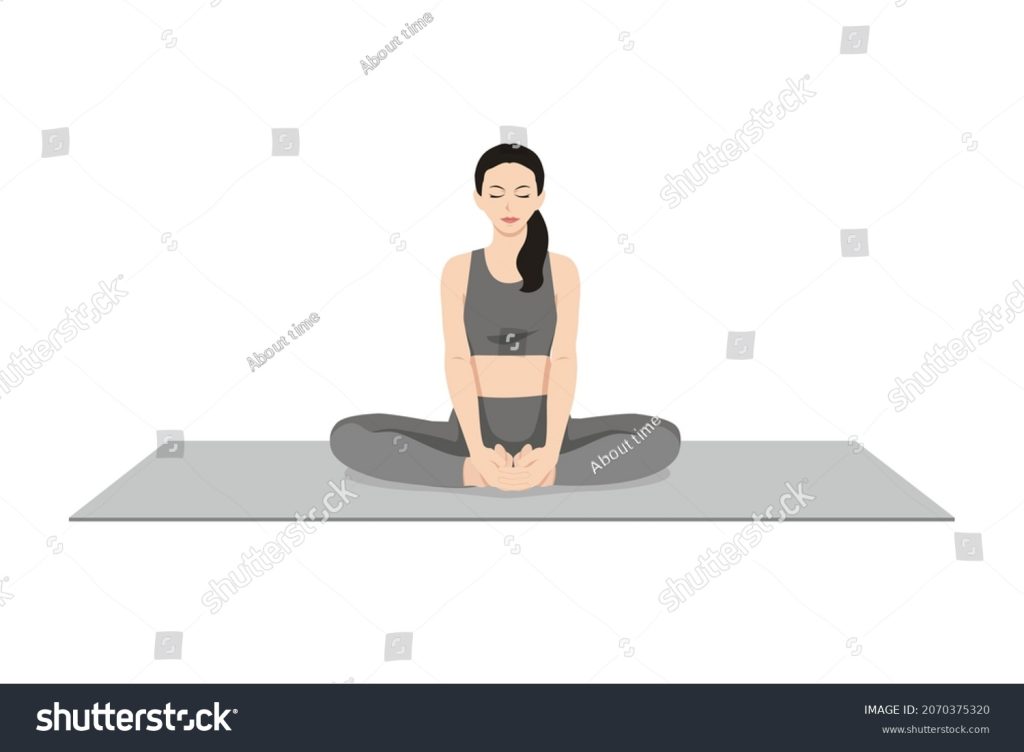
Baddha Konasana (Bound Angle Pose)
- Promotes circulation in the lower body.
- Stimulates abdominal organs.
- Stretches the inner thighs and groins.
- Reduces fatigue and improves posture
- Strengthens Pelvic Floor Muscles
Remember, always practice yoga under the guidance of a certified instructor and ensure that the postures don’t strain your body, especially when dealing with specific health conditions such as CVI.
References:
https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-venous-insufficiency
https://www.ahajournals.org/doi/10.1161/circulationaha.113.006898
https://www.ncbi.nlm.nih.gov/books/NBK430975/
https://pmc.ncbi.nlm.nih.gov/articles/PMC7173720/
https://pubmed.ncbi.nlm.nih.gov/10667639/
https://www.sciencedirect.com/science/article/pii/S1078588410006246
https://pubmed.ncbi.nlm.nih.gov/15230646/
https://www.1mg.com/generics/calcium-dobesilate-211353
https://synapse.patsnap.com/article/what-is-naftazone-used-for
https://go.drugbank.com/drugs/DB13680
https://www.drugs.com/international/naftazone.html
https://my.clevelandclinic.org/health/treatments/23211-phosphodiesterase-inhibitors
https://www.ncbi.nlm.nih.gov/books/NBK559096
https://www.mims.com/philippines/drug/info/reparil-n%20gel
https://pmc.ncbi.nlm.nih.gov/articles/PMC6776292/
https://www.sciencedirect.com/science/article/pii/S0944711322006687
https://pubmed.ncbi.nlm.nih.gov/8919258/
https://pubmed.ncbi.nlm.nih.gov/17484814/
https://my.clevelandclinic.org/health/diseases/16872-chronic-venous-insufficiency-cvi
https://www.rxlist.com/supplements/mesoglycan.htm
https://pmc.ncbi.nlm.nih.gov/articles/PMC2989756/
https://www.researchgate.net/publication/16006096_Glycosaminoglycans_from_pig_duodenum
https://my.clevelandclinic.org/health/treatments/23449-compression-therapy
https://www.sciencedirect.com/topics/nursing-and-health-professions/compression-therapy
https://pmc.ncbi.nlm.nih.gov/articles/PMC4081237/
https://theveininstituteofhunterdon.com/ambulatory-phlebectomy-its-not-vein-stripping/
https://my.clevelandclinic.org/health/treatments/6763-sclerotherapy
https://pubmed.ncbi.nlm.nih.gov/11081989/
https://www.ahajournals.org/doi/10.1161/circ.150.suppl_1.4142743
https://www.phytojournal.com/archives/2024/vol13issue5/PartF/13-5-62-708.pdf
