Warts
Warts are benign or noncancerous skin growths caused by the human papillomavirus (HPV). They’re most common on hands, feet, and even the face, but they can show up anywhere on the body. They affect people of all ages but are more common in children and young adults. Though they may be bothersome or persistent, they are generally harmless and often resolve on their own.

Overview
Warts are small growths on the skin caused by a viral infection, specifically by one of the many types of human papillomavirus (HPV). Although warts can appear anywhere on the body, they are most commonly found on the hands, feet, and face. They are usually skin-colored and rough to the touch but can also be dark, flat, and smooth. Warts are contagious and can spread through direct contact with someone who has them or through contact with a surface that has been touched by someone with warts. Sharing personal items such as towels, razors, or shoes can also spread the virus. Cuts or breaks in the skin can increase the likelihood of infection.
Types and Symptoms of Warts
Warts are classified based on their appearance and location on the body. Untreated warts can spread, cause pain, infection, bleeding, and cosmetic concerns, and, in the case of HPV-related warts, increase the risk of cancer and transmission to others.

The common symptoms of warts may include:
- A small, fleshy, grainy bump.
- The presence of tiny, clotted blood vessels that appear as dark dots at the wart’s center (“seeds”).
- In some cases, itchiness or mild tenderness.
| Type | Description | Prognosis | Symptoms |
|---|---|---|---|
| Common Warts | Typically found on fingers & hands. Common warts are skin-colored, rough, raised bumps, often grayish-brown, and feature a pattern of tiny black dots (clotted blood vessels). They can resemble a small cauliflower. | Typically harmless and may disappear on their own, though they can take months or years to resolve. | Rough, raised bumps Grayish-brown color Grainy appearance Tiny black dots |
Plantar Warts | Located at the bottom of the feet, especially heels and weight-bearing areas. Plantar warts can be painful when walking or standing due to their location, and they are often flat and have a hard central core. | May disappear without treatment but can be persistent and require intervention. | Hard, thick patches of skin A callus-like surface Pain or tenderness when walking or standing Flat growths on the sole of the foot |
| Flat Warts | Commonly found on the face, neck, hands, wrists, knees, and legs. Flat warts are smaller and smoother than other types, often appearing in clusters of 20-100, and are more common in children and teens. They are small, flat, and can be pink, brown, or yellowish. | Often disappears within months, especially in children. | Flat, smooth, and slightly elevated Smaller than other warts Pink, brown, or yellowish color Occur in clusters |
| Filiform Warts | They’re common on the face and neck. These have a distinct appearance, featuring long, narrow projections resembling tiny fingers that grow quickly. | They are likely to require treatment due to their prominent and inconvenient locations. | Long, narrow growths Flesh-colored Grow rapidly Appear on the face, around the eyes and mouth |
| Periungual Warts | These warts form around fingernails and toenails and can affect nail growth and cause nail deformities and pain. It is common in people who bite their nails. | They can be stubborn and might require medical treatment if affecting nail health. | Rough, irregular bumps Clusters around nails May affect nail growth Can be painful |
Genital Warts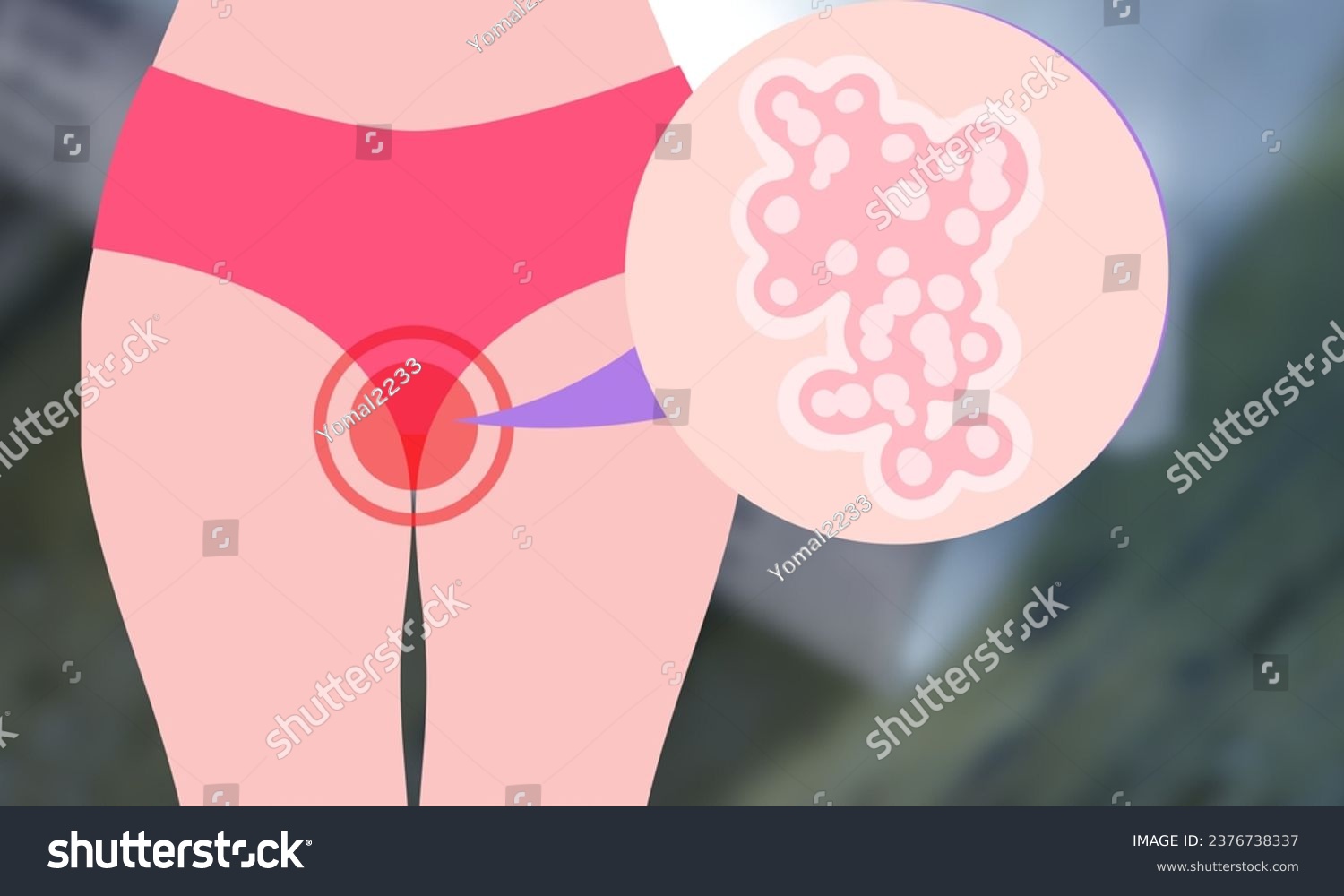 | These are generally specific to genital areas and are caused by certain strains of the human papillomavirus (HPV). They are a sexually transmitted infection. | Treatment can alleviate symptoms, but the virus may remain in the body. | Small, flesh-colored bumps Clustered appearance Can be itchy or discomforting Occur in the genital region |
When to See a Doctor
While warts are usually harmless, they can sometimes lead to complications, especially if left untreated or if they occur in sensitive areas. See a doctor if you experience:
- Pain and Discomfort: Plantar warts can make walking painful, while periungual warts may affect nail growth.
- Bleeding and Infection: Scratching or injuring a wart can lead to infection, causing redness, swelling, and pus, especially in those with weak immune systems.
- Spreading to Other Body Parts: Warts can spread to other body areas through touching, scratching, or shaving.
- Recurrence and Persistence: Some warts persist or return despite treatment, particularly in those with weaker immune systems.
- Sensitive Areas: Warts on the face, genitals, or under the nails should always be evaluated.
- Potential Malignancy: In rare cases, certain wart types may require further evaluation.
- Infection Signs: Redness, swelling, pus, or warmth around the wart.
- Weakened Immune System: If you have a condition like diabetes, HIV, or are undergoing immunosuppressive treatment
Special Cases
- Weakened Immune System: Warts may be harder to treat; monitor closely for infection or unusual growth.
- Pregnancy: Genital warts may be treated with cryotherapy and often disappear after childbirth, but it is advisable to follow up with your doctor for preventive measures.
Doctors to Consult
- Dermatologist: A skin specialist for persistent, recurring, or complicated warts.
- General Physician: Can assess, diagnose, and treat mild to moderate cases or refer to a specialist if needed.
- Podiatrist: Specializes in foot care, useful for plantar warts that cause pain or walking difficulties.
- Pediatrician: Manages warts in children, including common and plantar warts.
- Psychologist: Can help if visible warts cause emotional distress or impact self-confidence.
- Oncologist: Evaluates and manages HPV-related cancers, such as cervical, anal, or throat cancer.
Note: While an oncologist is not typically consulted for common warts, referral may be necessary if there are concerns about malignancy or HPV-related complications.
Risk Factors/Causes
Individual Factors
- Age: Children and young adults are more susceptible.
- Immune Status: People with weakened immune systems, such as those with HIV/AIDS or who have had organ transplants, are at higher risk.
- Skin Conditions: Conditions like eczema that leave the skin vulnerable and exposed increase the risk.
Behavioral Factors
- Nail Biting and Picking: These habits can cause breaks in the skin, facilitating the virus’s entry.
- Walking Barefoot in Public Areas: This increases the risk of contracting plantar warts.
- Occupational Exposure: Handling raw meat frequently, such as in a butchery, raises the risk.
- Tight shoes: Wearing tight shoes can contribute to the development and worsening of plantar warts (warts on the soles of the feet) due to increased friction & pressure.

Environmental Factors
- Communal Facilities: Using communal showers, locker rooms, or pools can increase the risk of exposure to the virus.
- Shared Personal Items: Sharing towels, razors, or other personal items with someone who has warts can lead to transmission.
Other Factors
- Smoking: It has been found to increase the risk of recurrence after successful treatment of warts.
- Genetic predisposition: Some people are naturally more prone to warts.
- Excessive sweating (hyperhidrosis): Creates a moist environment that helps HPV thrive.
- Delayed immune response in some individuals: Some people’s immune systems fail to recognize and clear the virus efficiently.
Prevention of Warts
Preventing warts involves a combination of good hygiene practices, lifestyle changes, and vaccination. Here are some effective measures to reduce the risk of developing warts:
General Hygiene and Lifestyle Measures
- Avoid Direct Contact: Do not touch warts on other people’s skin. If you do come into contact with a wart, wash your hands thoroughly with soap and water. Do not pick at warts, as this can spread the virus to other parts of your body.
- Protect Your Skin: Keep your skin clean and moisturized to prevent it from becoming dry and cracked. This helps to create a barrier against the virus.
- Avoid Biting Nails and Picking Cuticles: These habits can create breaks in the skin, making it easier for the virus to enter.
- Cover Warts: If you have a wart, cover it with a bandage to prevent it from spreading.
- Wear Protective Footwear: Wear flip-flops or shoes in public locker rooms, pool areas, and showers to avoid contact with the virus.
- Maintain a Strong Immune System: A healthy diet, adequate sleep, and stress management can help boost your immune system, making it more effective at fighting off the virus.
Sexual Health Measures
- Use Condoms: While condoms can reduce the risk of transmitting genital warts, they do not provide complete protection as the virus can infect areas not covered by the condom.
- Limit Sexual Partners: Reducing the number of sexual partners and avoiding sexual activity with individuals who have visible genital warts can lower your risk.
- HPV Vaccination: The HPV vaccine can prevent infection with certain types of HPV that cause genital warts and related cancers. It is recommended for children and young adults, typically ages 9 to 26.
Additional Tips
- Avoid Sharing Personal Items: Do not share towels, washcloths, clothing, nail clippers, or razors with others.
- Practice Good Hygiene in Public Spaces: Be cautious in communal areas like gyms and swimming pools, and avoid touching surfaces that may be contaminated.
Diagnosis
Warts are primarily diagnosed through clinical examination, with additional laboratory tests used if needed.

Clinical Examination
- Visual Inspection: During the examination, the doctor visually assesses the wart’s appearance, noting its size, shape, and color. This helps determine the type of wart, such as common, plantar, flat, filiform, or genital.
- Palpation (Touch Examination): The doctor then uses palpation to evaluate the texture, thickness, and mobility of the wart. This helps differentiate it from other skin conditions like calluses, corns, or skin tags.
- Key Signs: Important signs to look for include:
- Interrupted skin lines
- Presence of black dots, which are thrombosed capillaries
- No pain unless pressure is applied (commonly seen in plantar warts)
Diagnostic Tests
If the clinical diagnosis is uncertain, additional tests can be performed:
- Dermoscopy (Skin Surface Microscopy)
Magnified skin inspection revealing thrombosed capillaries, papillomatosis (a characteristic pattern of skin growth), and keratotic structures (areas of thickened skin). - Acetowhite Test (For Genital Warts): The acetowhite test involves applying acetic acid to the genital area. This causes HPV-infected areas to turn white, making them easier to identify during diagnosis.
- Colposcopy is used as a follow-up to further examine any suspicious areas identified by the acetowhite test. A colposcope provides a magnified and detailed view of the genital area, allowing for a closer inspection of potential growths. This procedure helps in diagnosing conditions such as genital warts and can lead to biopsies if necessary.
- Skin Biopsy: A skin biopsy is recommended when a wart appears atypical, showing unusual features such as an irregular shape, color, or ulceration. It is also performed if there is a suspicion of skin cancer, such as squamous cell carcinoma. It involves examining a small tissue sample under a microscope, which can reveal:
- Hyperkeratosis (thickened outer layer of skin)
- Papillomatosis (finger-like projections)
- Viral inclusions (abnormal structures within cells caused by viral infections)
- Polymerase Chain Reaction (PCR) for HPV DNA: Detects the presence and subtype of HPV, particularly useful in persistent or high-risk cases associated with cancer.
- HPV Typing (Genotyping): Identifies specific HPV strains to assess cancer risk, especially in genital warts.
- Blood Tests (Rarel): Occasionally used to evaluate immune function in immunocompromised patients, as persistent warts may suggest weakened immunity.
Differential Diagnosis
Warts can mimic other skin conditions, so tests may be needed to rule out the following:
| Condition | Key Differences from Warts | Diagnostic Test |
|---|---|---|
| Calluses/Corns | No black dots; skin lines remain intact | Clinical exam |
| Molluscum contagiosum | Central dimple, pearly appearance | Biopsy, PCR |
| Skin Tags | Soft, pedunculated (on a stalk) | Clinical exam |
| Seborrheic Keratosis | Waxy, stuck-on appearance | Dermoscopy, biopsy |
| Squamous Cell Carcinoma | Ulceration, bleeding, rapid growth | Biopsy |
Warts are mainly diagnosed clinically, but dermoscopy, biopsy, PCR, and HPV typing help confirm cases. In genital warts, acetowhite testing and HPV DNA analysis are particularly useful. Biopsy is recommended for atypical or treatment-resistant lesions.
Allopathic Treatment
Allopathic treatment for warts involves a variety of medical interventions aimed at removing the wart and preventing its recurrence. The choice of treatment depends on the type, location, and severity of the wart, as well as the patient’s age and overall health.
First-Line Treatments
Common and Plantar Warts Treatment
Salicylic Acid (Keratolytic Agent)
Salicylic acid softens and removes thickened skin layers of warts. Available as liquids, gels, and plasters, it requires daily application after soaking the wart in warm water. Treatment may take weeks to months, with a 70–80% success rate.

Cryotherapy(Freezing)
Cryotherapy involves applying liquid nitrogen to freeze and destroy wart tissue, forming a blister that falls off within 1-2 weeks. It requires multiple sessions and has a 50-70% success rate, with potential side effects like pain, blistering, and skin discoloration.

Cantharidin (“Blister Beetle Extract”)
A doctor-applied blistering agent that forms a blister under the wart, causing it to fall off in about a week. May result in scarring.
Genital Warts Treatment
Podophyllin and Podofilox
Used for genital warts, these treatments stop cell growth and destroy wart tissue. Podophyllin is applied by a doctor, while Podofilox can be used at home. Not recommended during pregnancy.
Topical Imiquimod (Aldara, Zyclara)
Imiquimod boosts the immune system to fight HPV and is effective for genital and large warts. Applied three to five times weekly for several months.
Second-Line Treatments
Laser Therapy
Laser therapy targets the wart’s blood supply using a pulsed-dye or CO2 laser, causing the wart to shrink and fall off. It’s ideal for large, deep, or resistant warts and has a success rate of 70-90%, with potential side effects like pain, scarring, and pigmentation changes. Effective for both cutaneous and genital warts, particularly those on the hands, feet, and face.
Surgical Excision/ Electrosurgery and Curettage
Surgical excision removes warts down to the dermal-epidermal junction. These treatments, done under local anesthesia, are effective for resistant warts, with an 80-90% success rate. However, risks include pain, scarring, and possible recurrence. Recommended for stubborn common warts, filiform warts, and plantar warts. Commonly used techniques include:
- Electrosurgery uses an electric current to burn the wart.
- Curettage scrapes it out with a sharp instrument.
- Tangential scissor excision and shave excision involves removing a superficial skin lesion by making a shallow, parallel cut to the skin surface using fine scissors or a scalpel.
Topical Retinoids
Retinoids (e.g., Tretinoin) slow wart cell growth, leading to regression. They work best for flat warts, especially when other treatments fail. Start with the lowest strength and apply a pea-sized amount to affected areas.
Duct Tape Occlusion Therapy
The exact mechanism is unclear; it may stimulate an immune response or break down the wart tissue. Cover for six days, then remove, soak, and debride. Repeat as needed. Effectiveness varies but mainly used to treat common warts in hands and feet.
Third-Line Treatments
- Immunotherapy stimulates the body’s immune system to fight recalcitrant or widespread warts. Common immunotherapy options include
- Topical Immunotherapy
- Imiquimod (Aldara, Zyclara): A topical immune response modifier used for genital warts, common warts, and flat warts.
- Diphenylcyclopropenone (DPCP): Applied to trigger an allergic reaction, stimulating the immune system.
- Squaric Acid Dibutyl Ester (SADBE): Causes mild irritation to recruit immune cells to fight warts.
- Intralesional Immunotherapy (Injections into the Wart)
- Candida Antigen: Injected into warts to provoke an immune response, effective for multiple warts.
- Mumps or Trichophyton Antigen: Similar to Candida antigen, stimulating immunity.
- Interferon-alpha: Boosts immune response but is used less frequently due to side effects.
- BCG Vaccine: Used off-label to enhance immune response in stubborn warts.
- Topical Immunotherapy
These treatments are considered for resistant, extensive, or recurrent warts, especially when conventional therapies fail.
- Chemotherapy drugs are sometimes used for recalcitrant, extensive, or high-risk warts, particularly those resistant to standard treatments. These drugs work by inhibiting viral replication or disrupting abnormal cell growth.
- 5-Fluorouracil (5-FU) (Efudex, Carac)
Is a topical antimetabolite chemotherapy that inhibits DNA synthesis. It is used to treat anogenital warts, plantar warts, and stubborn cutaneous warts and applied topically under medical supervision. For improved effectiveness, it is often combined with salicylic acid to enhance penetration. May cause redness, irritation, and peeling. - Bleomycin
Is a cytotoxic antibiotic injected directly into resistant warts, disrupting cell growth and triggering an immune response. It is sometimes used off-label for stubborn or treatment-resistant warts, particularly plantar and deep-seated warts. Side effects may include pain, necrosis, scarring, and potential nail damage when applied to fingers or toes.
- 5-Fluorouracil (5-FU) (Efudex, Carac)
- Oral Medications help boost the immune response or inhibit viral replication and are typically prescribed for extensive or treatment-resistant warts only.
- Cimetidine (Tagamet): Used off-label to enhance immune response against the wart virus.
- Retinoids (Acitretin, Isotretinoin): Vitamin A derivatives that slow skin growth, used for widespread warts, especially in immunocompromised patients or for treating recalcitrant warts.
- Interferon: Helps manage extensive wart infections.
Which Treatment is Best?
| Wart Type | Best Treatments |
|---|---|
| Common Warts (Hands, Fingers) | Salicylic Acid, Cryotherapy, Electrosurgery |
| Plantar Warts (Feet) | Salicylic Acid, Cryotherapy, Laser, Immunotherapy |
| Flat Warts (Face, Legs) | Retinoids, Imiquimod, Cryotherapy |
| Genital Warts | Podofilox, Imiquimod, TCA, Laser, HPV Vaccine |
| Resistant Warts | Laser, Electrosurgery, Immunotherapy |
Lifestyle Changes for the Management of Warts
Warts are caused by certain strains of the human papillomavirus (HPV). While they can be stubborn, certain lifestyle changes may help manage them and potentially reduce their occurrence.
- Maintain Good Hygiene:
- Wash your hands regularly, especially after touching warts, to prevent spreading.
- Avoid picking or scratching at warts to prevent further infection or spreading.
- Avoid Direct Contact:
- Avoid direct contact with warts on other people or sharing personal items like towels, razors, or footwear.
- Keep Skin Moisturized:
- Use moisturizing lotions to keep skin healthy, as dry or cracked skin may be more susceptible to infection.
- Boost Your Immune System:
- Eat a healthy, balanced diet rich in vitamins and minerals to support immune function.
- Engage in regular physical activity and ensure adequate sleep.
- Protect Your Feet:
- Wear flip-flops or shoes in communal areas like pools, locker rooms, or showers to avoid plantar warts.
Allopathic Supplements and Treatments
Several treatments and supplements may aid in managing warts:
- Vitamin A: Topical application has shown promise in treating persistent warts by supporting skin health and immune function.
- Vitamin C: Vitamin C is vital for immune support and skin health. Higher vitamin C intake may be linked to a reduced risk of persistent HPV infection, though more research is needed.
- Retinoids: Topical agents that promote skin cell turnover; may help reduce wart growth.
- Zinc Sulfate: Boost immune response against HPV; some studies show positive results but require caution with long-term use. May aid in treating viral warts.
Recommendations
Individualized Approach: Treatment should be tailored to the individual, considering factors like the type of wart, location, size, and the patient’s overall health.
Consultation: Always consult with a doctor before beginning any new treatment or supplement, especially if you have persistent or large warts or if they cause discomfort.
Medication/Drugs
| Medication/Drug | Class | Mechanism of Action | Side Effects | Brand Names in India |
|---|---|---|---|---|
| Salicylic Acid | Keratolytic Agent | Dissolves the substance that causes skin cells to stick together, encouraging the shedding of skin layers. | Skin irritation, burning sensation, dry skin | Salicylix SF (salicylic acid ointment), Medisynth Wartex Cream, Salactin Salicylic & Lactic Acid Paint |
| Podophyllin & Podofilox | Antimitotic Agent | Affects the growth of skin cells and slows the growth of warts. | Skin irritation, burning, inflammation | Podowart, Condyline Solution, Podowart Paint (Podophyllin) |
| Imiquimod | Immunomodulator | Stimulates the immune system to produce interferon and other cytokines to attack the warts. | Redness, swelling, itching, burning | Aldara, Imiquad, Qmica |
| Cantharidin | Vesicant Agent | Causes blister formation, lifting wart from the skin. Note: This procedure should be performed in a doctor’s clinic or hospital under proper medical supervision. | Blistering, pain, redness | Ycanth (Cantharidin) Note: Not widely available in India. |
| 5-Fluorouracil (5-FU) | Antimetabolite/ Chemotherapy drug | Inhibits DNA synthesis and cell division in rapidly dividing cells. Note: If injection, then can only be administered by doctors. | Skin irritation, redness, peeling | Oncourcil 250mg, Flonida 5% Cream, Efudex – Fluorouracil Cream 5% USP |
| Bleomycin | Cytotoxic antibiotic/ Chemotherapy drug | Inhibits wart cell growth and triggers an immune response. These are injected into the wart. | Pain, necrosis, scarring, possible nail damage | Bleochem, Bleocip |
| Topical Retinoids | Retinoids (Vitamin A derivatives) | Retinoids disrupt the cell growth of warts. They may be the best treatment for flat warts on the back of the hands. Creams may need to be used for a few months before warts disappear. | Skin dryness, Peeling, Redness, Irritation or burning sensation | (Acitretin – oral) A-Ret 0.1% Gel, Retino A Micro 0.1% Gel (Adapalene) Adaferin Gel, Adapalene Gel 0.1% (Isotretinoin – Topical) A Ret 0.025% Gel, Acnon 0.025% Gel |
| Cimetidine (Oral) | H2 Receptor Antagonist (H2 blocker) | Cimetidine, an H2-receptor antagonist, is believed to boost the immune response against HPV by enhancing T-cell activity; it is used off-label though its effectiveness for warts is debated. Drug Interactions: Can inhibit liver enzymes (CYP450), affecting the metabolism of various drugs (e.g., warfarin, phenytoin). | Headache, diarrhea, dizziness, Headache, Fatigue Hormonal Effects (with long-term use): Gynecomastia (breast enlargement in men), Decreased libido, Irregular menstrual cycles in women | Tymidin, Ulciban, Tagasec, Tymidin, Cimetiget |
| Oral Retinoids | Retinoids (Vitamin A derivatives) | Oral retinoids, like isotretinoin, treat acne by reducing sebum production, regulating cell turnover in hair follicles, and decreasing inflammation. They work by binding to nuclear receptors, altering gene expression, and normalizing the abnormal keratinization process that causes acne. | Dry skin, lips, and eyes; sensitivity to sunlight; headache; muscle or joint pain. Some severe cases might have: Liver damage, depression, mood changes, birth defects (teratogenic), high cholesterol, and blood sugar levels. | (Isotretinoin): Sotret, Isotroin (Acitretin): Acipsor, Zoratame |
Ayurvedic Treatment
Ayurvedic Approach
In Ayurveda, warts can be compared with “Charmakeela” or “Charmakila”. The diagnosis is based on clinical examination and is usually straightforward by visual inspection. It is caused by a Vata-Kapha imbalance, leading to abnormal skin growth. The features or types depend on the dominant dosha:
- Vata causes dryness and tissue growth.
- Kapha promotes thickening and accumulation.
- Pitta may add inflammation.
- Srotas Involvement:
- Affects Rakta (blood), Mamsa (muscle), and Twak (skin) Dhatus, disrupting metabolism.
- Rakta Vaha Srotas blockage impairs circulation, promoting wart formation.
Ayurveda prescribes oral medications, topical use of Kshara (alkaline ash of herbs), Agni (thermal cautery), and Shastra Karma (surgery) for removal of Charmakila.
Ayurvedic Treatment Procedures:
Ksharasutra (thread smeared with Kshara) Therapy: A medicated thread coated with Apamarga Kshara is tied around the wart, cutting off blood supply and leading to its removal. Medicated horse hair can also be used, particularly for filiform warts.
Agnikarma (Thermal Cauterization): Uses heated metallic rods (Shalaka) to burn off stubborn warts while ensuring surrounding skin remains unharmed. Effective for common, filiform, plantar, and genital warts.
Apamarga Kshara (Achyranthes Aspera): A potent alkaline herbal extract prepared from the ash of Achyranthes Aspera, applied topically for controlled wart destruction. Requires multiple sessions for complete removal.
Lekhana karma (scraping procedure): A paste of lime and copper sulfate is applied to the wart for five minutes before scraping it off with a betel leaf stalk (Piper betle, Linn.). The area is dressed with turmeric powder on day one and Jatyadi Taila on following days. Effective for common and filiform warts.
Changeri Leaf Paste (Oxalis Corniculata): Fresh Changeri leaves are ground into a paste and applied to the wart. Their anti-inflammatory and antimicrobial properties help reduce wart size and promote healing, particularly for cosmetic and flat warts.
Dietary & Lifestyle Modifications
- Increase immunity-boosting foods like Amla, Tulsi, and Neem to fight HPV infections.
- Avoid excessive oily, cold, and heavy foods that aggravate Kapha dosha.
- Maintain skin hygiene and avoid scratching warts to prevent spread.
Herbal Remedies

These natural treatments use herbs with antiviral, antimicrobial, and/or healing properties to help remove warts.
- Garlic: Crush a clove, make a paste, apply to the wart, and cover with a bandage. Repeat daily for 3-4 weeks.
- Aloe Vera: Apply fresh gel directly to the wart, cover, and repeat daily until it disappears.
- Apple Cider Vinegar: Soak a cotton ball, secure it overnight, and repeat daily for a week. The acidic properties help dissolve the warts.
- Indian Gooseberry (Amla): Apply fresh juice, let it dry, rinse, and repeat daily.
- Castor Oil: Apply directly, cover, and repeat daily for 2-3 weeks.
- Turmeric: Make a paste with mustard oil or water, apply for 30 minutes, and wash off. Repeat twice daily. A mixture of turmeric, neem & tulsi can also be used.
- Onion Juice: Onion juice contains enzymes that can break warts and stimulate the immune system. Apply fresh juice, cover, and repeat daily until the wart disappears.
- Potato: Place a small piece on the wart, secure overnight, and repeat daily.
- Honey: Apply a small amount, cover overnight, and repeat daily.
- Lemon Juice & Onion: Apply lemon juice, cover with onion pieces for 30 minutes, and repeat for 3-4 weeks.
- Baking Soda: Dries out and exfoliates warts. Apply a baking soda-water paste, cover overnight, and repeat daily. Mix with castor oil or apple cider vinegar for better results.
- Tea Tree Oil/Castor Oil Compress: Both oils help in wart removal when applied regularly.
Ayurvedic Medicines
| Herbal Medication | Description | Brands |
|---|---|---|
| Krishna Jeeraka (Black Cumin) | Used for its immune-boosting and detoxifying properties. It is known to enhance digestion and overall health, which can support the body’s ability to fight infections. | Yamkay Karunjeeragam Capsules Black Cumin, Baidyanath Hingwashtak Churna |
| Haridra (Turmeric) | Applied topically for its anti-inflammatory and antiviral properties. Turmeric is a powerful natural remedy known for its ability to reduce inflammation and fight viral infections. | Dabur Haridra Khanda (Vrihat), Patanjali Curcumin Gold 95 |
| Jatyadi Taila | An herbal oil applied externally to help dry out and reduce warts. It is effective for treating wounds, burns, and skin infections and is known for its healing properties. | Baidyanath (Jhansi) Jatyadi Tel, Jathyadi Kera Tailam |
| Sariva (Hemidesmus indicus) | Used internally for blood purification and detoxification. It helps maintain a healthy immune system and supports overall well-being. | Baidyanath (Jhansi) Sarivadhyasava, Bharat Organic Anantamul |
| Chandana (Sandalwood) | Has cooling and anti-inflammatory effects when applied topically. | Chandanbala Lakshadi Tail |
| Ashwagandha (Withania Somnifera) | Boosts immunity and helps the body respond to infections. It is a powerful adaptogen that supports the immune system and helps in managing stress. | Ashwagandha Tablets, Baidyanath Ashwagandha Churna |
| Garlic Paste | Antiviral and antimicrobial properties help reduce warts. | Garlic Pearls Capsules, Dabur Lasunadi Vati |
| Vacha (Acorus calamus) | Used for its antiseptic and decongestant properties internally and externally. It helps in purifying the blood and supports overall health. | Vacha Churna |
| Arka (Calotropis Gigantea) | The latex from the plant is applied to dissolve warts gradually. | Arka Tail |
| Ayucar Labs, D-Wart Cream | The cream contains ingredients like aloe socotrina, antimonium crudum, collinsonia canadensis, dulcamara, graphites, ruta graveolens, sarsaparilla, and sulphur. | D-Wart Cream |
Key Considerations:
- Consultation: Always consult with an Ayurvedic practitioner before beginning any new treatment, especially if you have persistent or large warts or if they cause discomfort.
Siddha Treatment
In the Siddha system of medicine, warts are referred to as “Marul,” “Naimul,” or “Kondai.” They are believed to result from an imbalance of Vatham and Kaba humors, affecting Ranjagam and Prasakam of Pitham. Among the seven Udalthathukal, Saaram, Senneer, Oon, and Kozhuppu are impacted.
They are treated using various complex herbal and mineral formulations. The treatment plan often includes both external and internal medications to reduce the size of warts, improve immunity, and restore skin health.
Siddha Treatment Approaches
Motchai Patru (Dolichos lablab): This is commonly used in wart treatments due to its medicinal properties. The bean is believed to help in reducing warts through its anti-inflammatory and antimicrobial actions.
Suttigai (Cautery Cauterization): A cauterization technique using a heated instrument (Uloga Suttigai – Metal Cauterization) may be employed in certain cases to remove warts. This method involves applying heat to the wart to destroy the tissue and promote healing.
Siddha Medicines
The following table lists some of the Siddha medications used for treating warts:
| Medication | Formulation Type | Brands |
|---|---|---|
| Amirtha Vennai (external use) | It’s made of butter and mercuric chloride. It is used in treating various types of external ulcers and wounds. | SKM Amirtha Vennai |
| Sanga Thiravagam (external use) | It is a mineral preparation known for its antiseptic, anti-inflammatory, and detoxifying properties. When applied topically, it helps reduce acne by controlling excess oil secretion, reducing bacterial infections, and promoting skin healing. | IMPCOPS Sanga Dhiravakam |
| Parangipattai Chooranam | Parangippattai chooranam can be given in all types of skin diseases like leucoderma, blackening and thickening of skin and in syphilis. | Medisiddh Parangipattai chooranam |
| Wartosin | The product contains Khatika, Cuma, Spatigam, Tankana, Karpoor and Rose water. It is used for remove of elevated warts. | Wartosin Wart Remover |
| Chirattai Thailam | Chirattai is a Classical Siddha medicine, it is used to treat is a very effective medicine for all skin diseases. | SKM Chirattai Thailam |
| Kungiliya Vennai | Kungiliya Vennai, a paste of Sap tree resin and ghee, is applied to warts for its antiviral and skin-healing properties. | IMPCOPS Kungiliya Vennai |
| Mirutha Singi Kalimbu | It is used for treating genital warts. Mirutha Singi also called as Massicot or Litharge in English is a mineral extracted from mines and also synthesized using Modern Methods. | |
| Parangipattai Kudineer | It can be used internally or externally with goat milk to reduce black markings and help skin conditions. | SKM Parangipattai kudineer chooranam |
| Nilavembu Kudineer | It is known to stimulate the immune system and prepare the body to fight against infections. It is also an effective remedy for allergies. It is all safe and healthy to consume in cases of HPV. Its antiviral antibacterial | KILLI Nilavembu Kudineer Chooranam Powder |
| Eladi Chooranam | Eladi choornam keeps the skin clear, bright and healthy and is used effectively in managing skin complaints like rashes, itching, dry and wet lesions | SKM Eladi Chooranam |
| Amukkara Chooranam | It is used to balance vata and Kapha doshas. These are effective in lowering physical and mental stress, restoring energy, | SKM Amukkara Chooranam |
| Gandhaga Rasayanam | Protects skin and connective tissues. | Dabur Gandhak Rasayan |
| Palagarai Parpam | Ayurvedic formulation crafted from a blend of herbs and minerals processed using specialized techniques for the skin disorders. | Medisiddh Gandhaga Parpam |
| Muthuchippi Parpam | Derived from pearl oyster shells, is sometimes used topically to treat warts due to its potential anti-microbial and skin-healing properties. | Impcops Muthuchippi Parpam |
| Ammanpacharisi milk (Euphorbia Hirta) – (external use) | Also known as asthma weed, is a plant that can be used to treat warts. The milky extract of the plant can be applied to warts to soften and remove them. | Saara HERBAL FRESH Amman Pacharisi Powder |
| Bramathandu milk (Argemone mexicana) – (external use) | Also known as Mexican poppy, Mexican prickly poppy. Seed oil, leaf juice and root are applied externally to relieve skin diseases and indolent ulcers like warts. | YOGIMATE Mexican Prickly Poppy Seeds Powder |
| Erukam paal (Calotropis Gigantea) – (external use) | Large shrub or small tree with milky sap that is also known as the crown flower or giant milkweed. It is native to India, Malaysia, Indonesia, and southern China. | Vedika Calotropis Gigantea Root Extract Powder |
| Pacha Karpoora Adai | Herbal Paste | Edible Pacha Karpoora Adai |
| Thirikadugam Chooranam | Herbal Powder | Medisiddh Thirikadugu Chooranam, SKM Thirikadugu Choorana |
| Kaalaani kalimbu | It is a popular Siddha cream used as chemical cauterization to remove hard skins, warts, corns, and skin tags, with the ingredients of limestone, arsenic tri-sulphuratum, copper sulphate, mercuric perchloride, lead sulfide, and bee wax. | Kalani Kalimbu Zigma |
| Chirattai kuzhi Thailam (external use) | Type of oil used to treat warts | SKM Chirattai Thailam |
It is crucial to consult with a qualified Siddha practitioner before using these treatments. They can tailor the treatment plan based on the individual’s specific condition and ensure the best possible outcomes.
Yoga
While yoga itself doesn’t directly cure warts, it can support healing by boosting immunity and reducing stress, which can help the body fight the HPV virus that causes warts. However, it is best to wear socks to prevent spreading of infectious warts. Here are some beneficial yoga practices:
Immune Boosting Poses
Viparita Karani (Legs-Up-The-Wall Pose)
Benefits: Promotes circulation and lymphatic drainage.
Bhujangasana (Cobra Pose)
Benefits: Strengthens the immune system and helps enhance blood flow, aiding in faster recovery of skin conditions.

Ustrasana (Camel Pose)
Benefits: Opens the chest and boosts immunity.
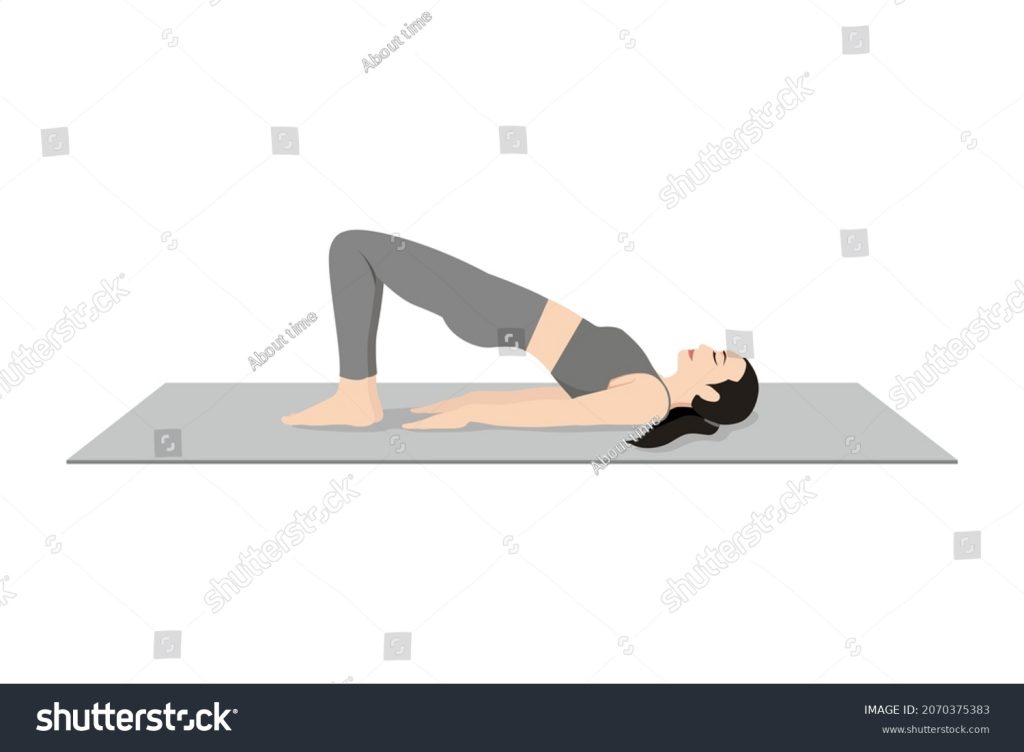
Setu Bandhasana (Bridge Pose)
Benefits: Supports lymphatic flow and detoxification.
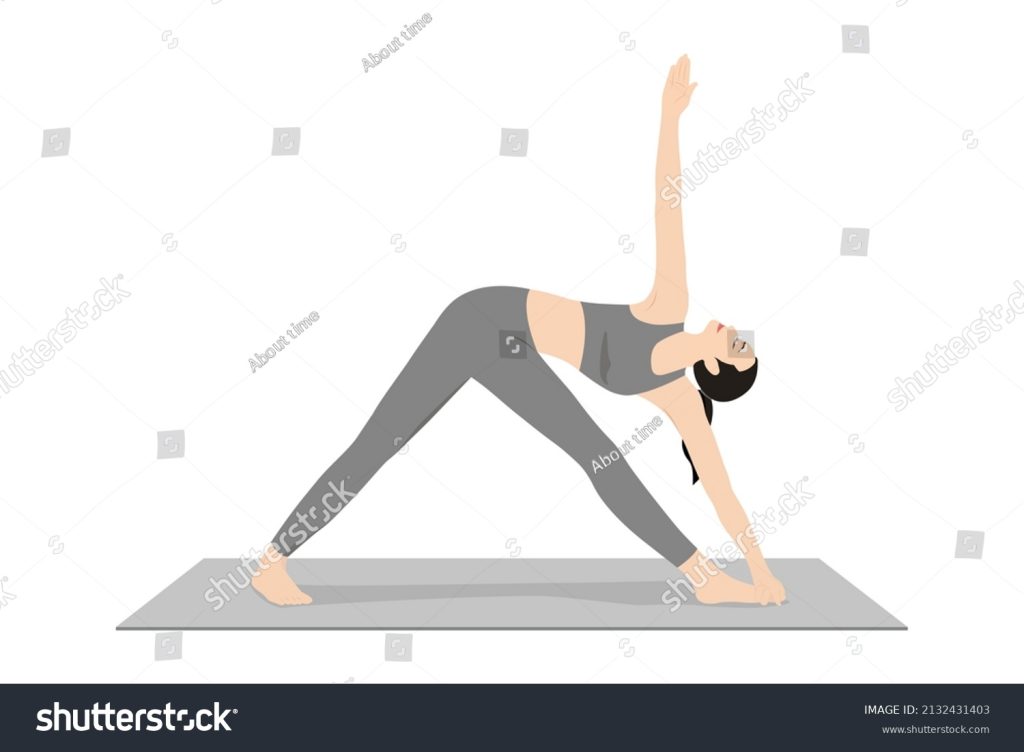
Trikonasana (Triangle Pose)
Benefits: Stimulates and improves blood circulation in the entire body, which can help rejuvenate skin health.
Tadasana (Mountain Pose)
Benefits: Improves blood circulation and helps in calming the mind, which supports overall health and healing.

Stress-Reducing Poses (Supports Healing)
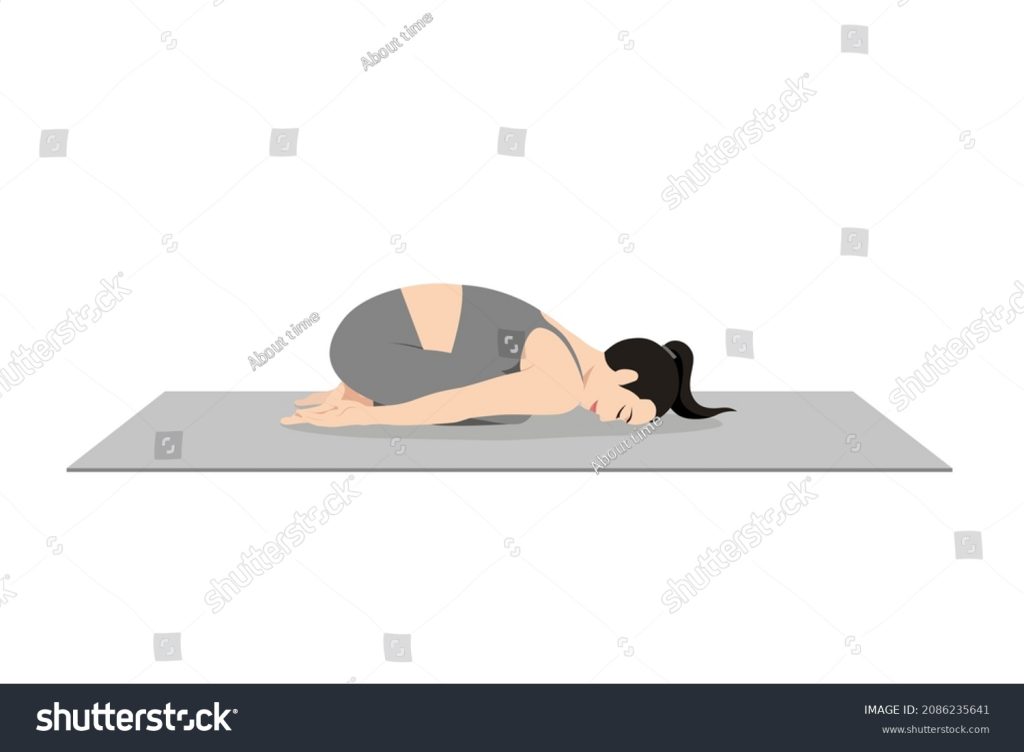
Balasana (Child’s Pose)
Benefits: This pose calms the nervous system and reduces stress.
Savasana (Corpse Pose)
Benefits: This pose encourages deep relaxation and recovery.

Sukhasana (Easy Pose) with Pranayama (Deep Breathing)
Benefits: Reduces stress and supports immunity.

While yoga can support wart healing, combining it with medical treatments (like salicylic acid or cryotherapy) will provide the best results. It is always recommended to consult with a doctor before starting any new exercise or treatment regimen, especially if you have persistent or large warts or if they cause discomfort.
References
https://journals.lww.com/aayu/fulltext/2011/32010/a_review_on_management_of_warts_in_ayurveda.19.aspx
https://www.truemeds.in/blog/natural-home-remedies-for-warts#Top_16_Effective_Home_Remedies_for_Warts
https://www.healthline.com/health/home-remedies-for-warts#from-the-kitchen
https://www.planetayurveda.com/library/home-remedies-for-wart/
https://www.researchgate.net/publication/51844188_A_review_on_management_of_warts_in_Ayurveda
https://www.alwaysayurveda.net/2017/05/periungual-warts-ayurvedic-treatment.html
https://pmc.ncbi.nlm.nih.gov/articles/PMC3215404/
https://emedicine.medscape.com/article/1133317-treatment
https://practicaldermatology.com/topics/general-topics/non-genital-warts-a-review-of-current-treatments/21884/
https://www.mayoclinic.org/diseases-conditions/common-warts/diagnosis-treatment/drc-20371131
https://my.clevelandclinic.org/health/diseases/4209-genital-warts
https://www.health.harvard.edu/diseases-and-conditions/how-to-get-rid-of-warts
https://www.webmd.com/sexual-conditions/hpv-genital-warts/hpv-treatment-is-there-hpv-cure
https://my.clevelandclinic.org/health/diseases/15045-warts
https://www.hopkinsmedicine.org/health/conditions-and-diseases/warts
https://pmc.ncbi.nlm.nih.gov/articles/PMC3215404/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4296436/
https://www.ayurvedjournal.com/JAHM_202061_04.pdf
https://lifelineherbal.com.au/treatments/warts-ayurvedic-alternative-herbal-treatment.html
